In this section:
View the sections on Standard Diets, Religious, Cultural, Personal and Lifestyle Considerations and Specific patient groups.
3. Therapeutic Diets
The details here are given so that any changes to the general standards can be considered and incorporated at the menu planning stage.
Therapeutic diets covered in this section:
3.1 Modified Texture
3.2 Finger Foods
3.3 Renal Suitable
3.4 Food Allergy
3.5 Gluten Free
3.6 Other Therapeutic Diets
3.6.1 Low FODMAP
3.6.2 Catering for Immune-supressed Patients (Previously Neutropenic)
3.6.3 Liver Disease (Decompensated)
3.6.4 Test or Investigation
3.1 Modified Texture
|
Diet |
Modified Texture |
|---|---|
|
Recommended Menu Code |
3 4 5 6 |
|
Menu Type |
À la carte menu |
|
Patient Group Suitability |
Patients with difficulty swallowing, also known as dysphagia. This can be associated with several conditions including:
|
|
Rationale for Diet |
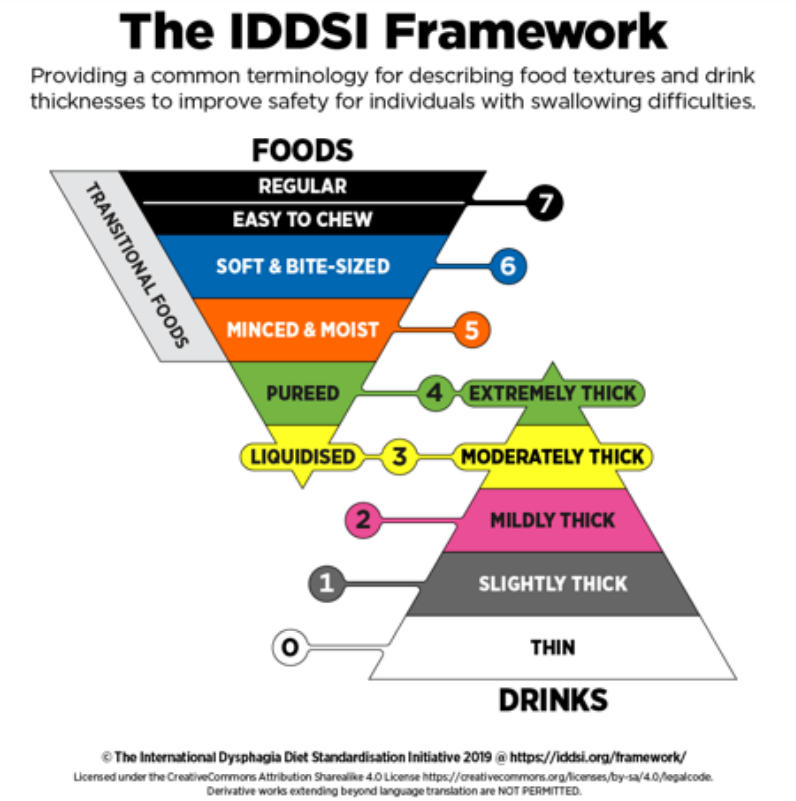
If dysphagia is not treated appropriately, it can result in choking, chest infections, dehydration, malnutrition and unintentional weight loss leading to negative health outcomes, poor quality of life and in some cases death. Texture modified diets are part of the multidisciplinary treatment of dysphagia. They are based on the IDDSI framework, which consists of a continuum of 8 levels (0 - 7), where drinks are measured from Levels 0 – 4 and foods are measured from Levels 3 – 7 (8). The IDDSI Framework provides a common terminology to describe food textures and drink thickness (6). |
|
Source |
We are grateful to the Food Services Specialist Group Committee for updating this section and the BDA Older People’s Specialist Group for their original contribution. |
Menu Planning Guidance
What are the IDDSI guidelines?
Always refer to the official IDDSI website for the most up to date framework, level descriptions, testing methods and resources: https://iddsi.org/
Hospital caterers need to ensure that patients have access to appropriate meals, snacks and drinks that meet both their nutrition requirements and their required consistency based on the IDDSI guidelines.
What levels do I need to cater for?
While the IDDSI guidelines recognise that it is safer for patients to progress through all the food texture levels in the framework (as appropriate), it is accepted that not all organisations will be able to offer all levels. Therefore, the levels offered should be agreed locally depending on the needs of the patients and in consultation with the Speech and Language Therapy team.
Best practice is to offer separate à la carte menus that cater for levels 3, 4, 5 and 6. The standard menu should contain regular level 7 foods with an adequate amount of easy to chew options as outlined in section 1.4 of this chapter (Easy to chew).
Special consideration should be given to menus for paediatrics as choking hazards in children differ to adults due to their smaller trachea size. Again, IDDSI have provided detailed guidance on their website.
What role does the Dietitian play?
People who are clinically at risk should be provided with a suitable menu after their assessment by a Speech and Language Therapist. It is the role of the dietitian to ensure that:
- Suitable choices are available, including snacks, to provide daily nutrient requirements
- Options fit the outlined budget
- Catering staff are adequately trained to provide suitable choices
- Processes are implemented to ensure required modified texture diets are communicated to catering staff
Can texture modified diets be made in house?
If the texture modified diet is produced in house, great care needs to be taken to ensure the consistency of the finished product is in line with IDDSI guidelines.
It is difficult to create uniform textures due to the variability of foods (e.g. fibrous vegetables versus cooked pasta), methods of processing and temperatures. Dietitians, speech and language therapists, nurses and caterers should work closely to ensure that people have access to the most appropriate and safe texture modified meals for their swallowing abilities.
If the consistency of the product cannot be guaranteed when produced in house, it may be necessary to purchase texture modified meals from a specialist provider whose meals comply with the IDDSI framework.
What breakfast and snack items are suitable for texture modified diets?
Any specific items should be tested in line with the IDDSI testing methods (16) and agreed locally with your Speech and Language Therapy team.
Some common food items that can be suitable for different texture modified diets include:
|
Texture Modified Diet |
Breakfast and Snack Options |
|---|---|
|
Level 3 Liquidised |
Smooth hot oat cereal or infant rice cereal made to the appropriate texture (requires clinical guidance), runny pureed fruit, moderately thick oral nutrition support drinks |
|
Level 4 Puree |
Smooth hot oat cereal or infant rice cereal made to the appropriate texture (requires clinical guidance), puree infant foods, thick yoghurt (no bits), custard, pureed fruit |
|
Level 5 Minced & Moist |
Smooth hot oat cereal or infant rice cereal made to the appropriate texture (requires clinical guidance), thick yoghurt (no bits), custard, pureed fruit, rice pudding |
|
Level 6 Soft & Bite Sized |
Smooth hot oat cereal or infant rice cereal made to the appropriate texture (requires clinical guidance), wheat biscuit completely softened in milk (where milk is fully absorbed), thick yoghurt (no bits), custard, pureed fruit, rice pudding, banana (cut into 1.5cm pieces) |
Please note: Transitional foods that change into a thin texture in the mouth may not suitable for people on a texture modified diet. These include ice cream, jelly, mousse and cream, whilst on thickened fluids.
3.2 Finger Foods
|
Diet |
Finger Foods |
|---|---|
|
Recommended Menu Code |
FF |
|
Recommended Menu Type |
À la carte menu or appropriate items coded on the standard menu |
|
Patient Groups Suitability |
Patients who have difficulty handling or recognising cutlery. This may include young children or patients with the following conditions:
|
|
Rationale for Diet |
Patients who find it difficult to use cutlery are at risk of not meeting their nutrition requirements, as they may be reliant on assistance with eating. Finger foods are foods that can be easily eaten by hand. Access to finger foods helps to prolong independent eating and allows patients to eat at their own pace, resulting in an improved oral intake for certain patient groups. Due to the benefits, the availability of finger foods for these patient groups in healthcare settings is included as a requirement in the Patient-Led Assessments of the Care Environment (PLACE) (17). |
|
Source |
Food Services Specialist Group (FSSG) |
Menu Planning Guidance
What needs to be considered when planning finger food options?
Adequate options that cover all meal components and snacks
Ensure there is a good variety of finger food options available for breakfast, main meals and snacks so that patients can meet their daily nutrition requirements. Avoid the main meal menu being only “party food” and include adequate vegetable and starchy side options to accompany the main component of lunch and supper meals.
Suitable textures
Dry foods can be obvious choices at mealtimes however they can lack the moistness and flavour of cooked products served in gravy or sauce. Alternatively, foods can’t be too messy to eat. Consideration of what foods are served with and the overall experience of eating a finger food meal is important.
Temperature
Cold and room temperature foods are quick and easy to serve and provide flexible snack options. Some main meal components need to be cooked before serving, which will need to work in line with the existing catering operations.
What are appropriate finger food ideas?
|
Breakfast |
Toast with spread cut into quarters, cereal bars, boiled eggs, mini sausages, omelette strips, cut up fresh fruit, drained tinned fruit, dried fruit, yoghurt in pouches or tubes |
|
Main meal component |
Chicken goujons, fish fingers, fish cakes, omelette strips, fish cakes, samosas, mini sausages, small kebabs or koftas, mini pies or sausage rolls, cold meat or smoked fish slices, boiled eggs, mini quiches or quiche fingers, spring rolls, pizza slices, dim sum, sushi, meatballs, falafel, sandwiches cut into quarters |
|
Side component for main meals |
Raw or cooked vegetable sticks or spears (e.g. carrot, peppers, broccoli, cauliflower, cucumber), cherry tomatoes, chips or potato wedges, boiled new potatoes, pitta bread wedges, cut up bread or rolls, crisps |
|
Dessert |
Mini fruit pies, cut up fresh fruit, drained tinned fruit, mini muffins, cake slices |
|
Snack |
Quartered sandwiches, cake slices, cold mini sausages rolls or pork pie, chopped fruit, dried fruit, cheese portions, crackers, biscuits, vegetable sticks with hummus, crisps, malt loaf or fruit bread with cream cheese or spread, scone with jam and spread |
More ideas can be found in the Caroline Walker Trust practical guide for supporting older people and older people with dementia (18).
What are the operational considerations when providing finger foods?
Hand hygiene
While hand hygiene is always important, processes and facilities that enable catering staff and patients to wash and sanitise their hands is crucial.
Preparation and presentation
Extra preparation is required when putting together finger food meals, whether it is done by a back of house catering team or at ward level. This can include removing packaging, cutting up foods, draining liquid or sauces and decanting. Catering staff may need further training to ensure they are plating and presenting finger food meals in an appealing and accessible way. For example, rolling up cold meats, slicing fruit into smaller pieces, quartering sandwiches and serving small pots of sauce.
Food safety
Care should be taken to serve hot finger foods at a comfortable/suitable temperature. While patients should be given adequate time to eat at their own pace, it’s also important to ensure high risk foods (e.g. sandwiches, cold meats) are not left out for too long.
3.3 Renal Suitable
|
Diet |
Renal Suitable |
|---|---|
|
Recommended Menu Code |
RS |
|
Recommended Menu Type |
Specialist à la carte menu or appropriate items coded on the standard menu |
|
Patient Groups Suitability
|
|
|
Rationale for Diet |
While there is no single ‘Renal Diet’, different dietary modifications may be necessary at different stages of kidney disease. Input from a specialist renal dietitian who has a good understanding of these patients’ dietary needs is essential. Patients with kidney disease may need to follow a diet that restricts any of the following:
Dietary restrictions will be dependent on the patient’s medical condition. Patients on renal dietary restrictions may need alternatives and additional snacks to meet their requirements. Many patients with kidney disease will be in the nutritionally vulnerable group due to the nature of their illness and possible renal-specific dietary restrictions. As kidney disease progresses, the risk of malnutrition also increases (19). Due to the variation of patients with kidney disease, it is important to consider age, ethnicity, length of stay, type of dialysis and the percentage of nutritionally compromised patients. Menus need to be designed to enable all patients to achieve a nutritionally complete diet within these constraints. Collaboration between caterers and specialist renal dietitians is crucial to meet the needs of this patient group. |
|
Nutritional Criteria for Diet Coding |
See Table 12.7 below. |
|
Source |
We are grateful to the BDA Renal Nutrition Specialist Group for their original contribution and revision of this section. |
|
Table 12.7: Recommended parameters for renal meals |
|||||||
|---|---|---|---|---|---|---|---|
|
|
Energy (kcal) |
Protein (g) |
Sodium (mg) |
Potassium (mg) |
Potassium (mmol) |
||
|
NW |
NV |
NW |
NV |
||||
|
Main meal |
300 |
500 |
12 |
21 |
644 |
1092 |
28 |
|
Dessert |
200 |
300 |
3 |
6 |
161 |
312 |
8 |
|
Total |
500 |
800 |
15 |
27 |
805 |
1404 |
36 |
NW = Nutritionally Well, NV = Nutritionally Vulnerable
Menu Planning Guidance
Protein requirements
The protein requirement for patients is based on their Ideal Body Weight (IBW) and will be a minimum of 0.8-1.0g protein per kg IBW. For patients on renal replacement therapies, requirements are in keeping with protein requirements recommended by SACN for the nutritionally vulnerable group of patients (1.1g/kg IBW/d) as listed in Chapter 9.
Therefore, menus should be based on meeting the nutrient targets provided in Chapter 9. Table 11.7 above provides details of the recommended nutritional parameters to be used when planning renal menus.
Additional protein items may need to be provided for vegetarians and vegans, those on fluid restrictions and renal replacement therapies. It is recognised that a large majority of renal patients will fall in the nutritionally vulnerable category, and menus should reflect this wherever possible.
40% of the protein requirements of the nutritionally vulnerable group are typically met by breakfast, snacks and milk (approximately 1 pint or 550mls in total = 20g protein). However, on a fluid restricted diet only ½ pint milk or 275mls is allowed, which causes a deficit of 10g protein. This deficit must be replaced and is best achieved by increasing the protein portion of the main meals. If this is not possible, for example where the protein portion of a plated meal cannot be increased, having milky puddings such as yoghurts, higher protein snacks, or the option of a cooked breakfast available, should be considered.
Potassium restrictions
Some patients will require a lower potassium diet. This will usually be the equivalent of 60-80mmols (or 2340-3120mg) per day, based on their IBW. Generally, the allowance is 1mmol potassium per kg IBW, but practice does vary.
Some vegetable and potato products may not be suitable depending on cooking methods. In general, cooking methods should leach rather than conserve potassium when preparing and cooking potatoes, fruits and vegetables. These items should be boiled before being offered to patients on a lower potassium diet. Local renal dietitians will advise on suitable low potassium cooking methods and dishes.
The availability of the estimated potassium content of dishes is necessary to allow accurate coding of the menu. The availability and accuracy of this information does pose challenges as suppliers are not required to declare this by law under the Food Information for Consumers (FIC) regulations. The potassium content information is likely to be calculated from food composition data tables due to expensive analysis methods. Nutritional analysis software can also be used – see Chapter 8 for some examples.
Salt substitutes containing potassium chloride should not be used.
Where poor appetite and potassium restrictions combine to make meeting requirements difficult, an à la carte menu allowing individualised choices may prove very helpful.
As a guide, to ensure suitable lower potassium main course options are available, meals should be planned with the aim to provide a maximum of 28mmol (1092mg) per main course and 8mmol (312mg) per dessert. The following table shows an example of how this can be broken down:
|
Table 12.8: Potassium Main Course Breakdown |
|
|---|---|
|
Meal component |
Example Potassium Content (mmol) |
|
Main |
<10 |
|
Vegetable side |
<8 |
|
Carbohydrate side |
<10 |
|
Dessert |
<8 |
|
Total meal |
<36 |
Mains with higher potassium levels can be served but ideally with lower potassium accompaniments, such as rice, pasta, or bread, as opposed to potatoes. The potassium content given above for vegetables is based on two 80g servings, i.e. 4mmol (156mg) from each serving. Regardless of the type or amount of carbohydrate or vegetables served, the priority should always be on ensuring the total meal does not exceed the maximum potassium recommendation.
Phosphate restrictions
Some patients will require a lower phosphorus diet to help control serum phosphate levels. Recommendations suggest that a low phosphorus diet should contain no more than 1400mg (45mmol) of phosphorus per day. However, this will often pose challenges for patients requiring a higher protein diet. Alternative high protein choices need to be provided to replace the following higher phosphorus foods when they are on the menu:
- Hard and processed soft cheese
- Kidney, liver
- Fish with edible bones
- Processed meats – e.g. ham, corned beef
- Chocolate
- Malted milk drinks
- Nuts
- Foods containing baking powder (e.g. scones).
Please note our reference to dietary phosphorus and serum phosphate. To avoid patient confusion around phosphorus and phosphate, dietary phosphorus is often referred to as phosphate in patient leaflets.
Salt intake
The aim for salt intake in renal disease is less than 6g day, which is in line with general guidance for salt intakes. If a higher salt option is on the menu, e.g. traditional curries, meat pies, sausage, ham or other processed items, it should be balanced by also offering menu choices lower in salt.
Renal day patients
Suitable dietary choices should be available for renal day patients where necessary (such as those on haemodialysis units), or in-patients requiring food outside standard mealtimes. Suggested suitable items would be:
- Sandwich with suitable filling (e.g., egg, tuna, chicken)
- • Fruit: apple, satsuma, drained tinned fruit
- • Plain cake or biscuit
- • Yoghurt or fromage frais
3.4 Food Allergy (hypersensitivity)
|
Diet |
Allergy |
|---|---|
|
Suggested Menu Type |
À la carte |
|
Patient Groups Suitability |
Patients with allergies (and/or intolerances) to any one or combination of the following:
Please note, the allergens listed above are those governed by UK foods laws (20). People may suffer from a food allergy not included in this list. |
|
Rationale for Diet |
UK food law Food allergies can be life threatening for individuals and must be taken seriously by food services. UK legislation requires all food services, including hospitals, to provide information about the presence of any of the 14 specified allergens in any of the food they serve to patients, staff or visitors. Caterers must also be able to evidence the exact ingredients used, including the brand names and pack sizes where applicable (this also includes any alternative ingredients used) (21). They must also take note of any precautionary ‘may contain’ labels on packaging. From 1 October 2021, the requirements for prepacked for direct sale (PPDS) food labelling changed in Wales, England and Northern Ireland. Also known as Natasha's Law, this labelling regulation helps to protect consumers by providing allergen information on the packaging (22). Any food business that produces PPDS food is required to label it with the name of the food and a full ingredients list. Allergenic ingredients must be highlighted within the ingredients list. Allergen management It is vital that information related to people’s food allergies is collected as early as possible and that it is communicated quickly and effectively to hospital caterers, ward staff and hospital dietitians. It is recommended that all healthcare facilities have a food allergy policy or a wider food and nutrition policy that includes allergen management. Allergen free menu To help cater to people with food allergies, it is recommended that hospitals have an ‘Allergen Free’ menu that is free from all 14 of the allergens governed by UK food law. This will help to minimise the risk of cross contamination and prevent patients from choosing an inappropriate option. Patients should also be free to choose from the standard menu and need to be provided with accurate allergen information to make a safe choice. |
|
Source |
We are grateful to The Anaphylaxis Campaign and allergy UK for their original contribution to this section. Thank you to the BDA’s Food Allergy Specialist Group for their feedback and comments to this edition. |
Menu Planning Guidance
What allergen information should be included on menus?
Information on menus should be kept to a minimum to reduce clutter and confusion. For this reason, allergen information should not be printed on standard menus for patients, instead include a statement on menus such as:
“Further information regarding food allergens is available upon request; please ask your Ward Host/Nutrition Assistant or Nurse”.
Allergen information for each menu item can be held in a separate matrix (hard copy and/or electronic) at ward level, so catering staff and clinical staff can determine meal suitability for patients with a food allergy or multiple allergies.
What is the responsibility of suppliers when it comes to allergen management?
It is vital that suppliers provide product specifications including the full ingredient lists that highlight any of the 14 allergens governed by UK food law. Failing that, the allergen information contained on the food labels can be used. Food labels should be checked on receipt into a facility to check that their allergens have not been changed.
All foodstuffs, from complete meals to individual recipe ingredients e.g. tomato sauce, breakfast cereals, that are brought into a hospital should have their ingredients checked and any of the 14 allergens identified, using either their specifications or food labels.
What is the responsibility of caterers when it comes to allergen management?
Food service staff should be proficient in allergen management, including the provision of allergen information, the risks of cross-contamination and cleaning methods. They should also understand the importance of effective food service systems to ensure the correct meal reaches the right patient. Information including online training can be obtained from the Food Standards Agency to support food service staff (23).
Some general tips for caterers include:
- Keep and refer to as necessary accurate and up-to-date ingredient lists from suppliers
- Have allergen management procedures in place in all steps of the food service pathway from receipt of ingredients to serving the patient with their meals
- If major allergens are included in a dish, the name of the dish should reflect this - refer to Food Standards Agency for guidance
- Major allergens should not be used where you would not expect to find them, for example, cashew nuts should not be used in pesto sauce or peanut flour in a curry.
How suitable is a ‘may contain’ statement for hospital catering?
Precautionary warnings for allergen labelling that food ‘may contain’ or is ‘not suitable for’ should only be used after a thorough risk assessment and the risk of cross-contamination cannot be eliminated or managed safely and poses a real risk to the patient. They should not be used as a substitute for good allergen management practices. If a product has a ‘may contain’ statement this information should be passed onto the patient. Further information regarding application of precautionary allergen labelling can be found on the Food Standards Agency website (24).
3.5 Gluten Free
|
Diet |
Gluten Free |
|---|---|
|
Recommended Menu Code |
GF |
|
Suggested Menu Type |
Standard or à la carte |
|
Patient Groups Suitability |
A gluten free diet is required for patients with:
|
|
Rationale for Diet |
A gluten free diet is the only medical treatment for coeliac disease and the skin condition dermatitis herpetiformis. In addition, some patients may request a gluten free meal to alleviate other health issues, for example gluten sensitivity, irritable bowel syndrome or they may have coeliac disease but not have a medical diagnosis. European regulation (Regulation (EU) No 828/2014) covers the labelling of gluten free foods and has been retained in UK law (25). It is applicable to foods served in catering facilities and all pre-packaged foods in the UK. By law, the term ‘gluten free’ may be applied only to food which has 20 parts per million (ppm) or 20 mg/kg or less of gluten. Making a gluten free claim for foods requires strict controls of ingredients, how they are handled and how they are prepared. A gluten free claim is a guarantee that the food is suitable for people requiring a strict gluten free diet. If there is any risk of cross contamination of a food or drink item at any stage, then the gluten free code should not be used for this item. For people with coeliac disease or dermatitis herpetiformis in a healthcare setting where their personal choice is restricted, a menu with gluten free choices that meets their nutritional needs must be made available. |
|
Source |
We are grateful to Norma McGough and Coeliac UK for their contribution to this section. |
Menu Planning Guidance
What is the safest way to provide gluten free meals to patients?
Depending on your food service system there are different options for catering to a gluten free diet, including:
Pre-packaged gluten free meal solutions
This may involve buying in a complete meal solution from a specialist dietary meals supplier or meals from regular suppliers that are labelled gluten free. Meals labelled gluten free must contain no more than 20ppm gluten. This also applies to all items on a menu, for example cereals, soups, yoghurts, desserts and biscuits.
Fresh cook meals
Depending on your production environment, you may be able to prepare gluten free meals in house to provide more choice for patients. Production of meals in a diet preparation area requires training of staff and separation of processes, equipment and ingredients. Meals can be produced with acceptable gluten levels of 20ppm or less when conditions and procedures are put in place to control cross contamination. Coeliac UK has produced guidance on preparing gluten free meals for caterers in collaboration with the Food Standards Agency (26).
Hospitals need to ensure that ingredients used to prepare gluten free meals do not contain gluten. Ingredient suppliers must provide you with information on the 14 allergens governed by UK food law in ingredients lists or product specifications for all the products you purchase from them. This includes cereals containing gluten. They should also follow Food Standards Agency guidance on communicating risk of contamination with allergens during manufacturing.
Can items on menus be identified as having no gluten containing ingredients?
Identifying individual meals as having ‘No Gluten Containing Ingredients’ (NGCI) on menus or using the ‘NGCI’ coding is not permitted. However, it is acceptable to produce a separate menu listing dishes that do not contain any gluten containing ingredients and where controls are in place to avoid cross contamination with gluten containing ingredients.
What policies are required to support the safe provision of a gluten free diet?
Healthcare establishments must:
- Have a written policy for providing gluten free meals. This should cover the meals and snacks available to patients requiring a GF diet, the menus available for patients to choose from and the controls in place to ensure GF meals and snacks are sourced, prepared and served to eliminate cross contamination
- Ensure a policy is in place to cover training for all staff involved in providing meals i.e. dietitians, front line food service assistants, catering and nursing staff
- Provide written materials for patients that help support informed choices and reflect the training of catering staff and the gluten free options available
What needs to be considered operationally to prevent cross contamination of gluten?
Care should be taken to ensure cross contamination does not occur at any stage of food preparation, for example:
- Gluten free bread must be toasted using a clean grill or toaster bags due to the risk of cross contamination
- If bulk multi-portion dishes are used, any meals from a supplier labelled as gluten free must be served with care to avoid cross contamination with other gluten containing foods
- Ensure separate utensils, probes and containers are used for gluten free foods where possible or that items are cleaned thoroughly between use
- Front line food service assistants, catering and nursing staff require adequate training to ensure they are competent in providing patients with a gluten free diet
3.6 Other Therapeutic Diets
The following diets may also require consideration depending on your type of healthcare facility and patient groups. It is best to consult with your Dietetics department to determine which type of catering solution would be best suited.
These solutions may include:
- A separate a la carte menu
- Coding on a standard menu
- Supplementary options that can be used together with a standard menu, e.g., an extra snack menu
- Alternative portion sizes of standard menu options
- Guidance to help create bespoke menus for individual patients, e.g., providing ingredient and nutrition information for each menu item
3.6.1 Low FODMAP
|
Diet |
Low FODMAP |
|---|---|
|
Patient Groups Suitability |
Patients with irritable bowel syndrome |
|
Rationale for Diet |
A low FODMAP (Fermentable, Oligosaccharides, Disaccharides, Monosaccharides And Polyols) diet is a diet restricted in short-chain fermentable carbohydrates and is often used for people with irritable bowel syndrome when general lifestyle and dietary advice have been trialled and symptoms still persist (27). A low FODMAP diet can be an effective treatment for gut symptoms such as bloating, abdominal pain and altered bowel habit. |
|
Menu Planning Guidance |
It is important to try and establish which stage of the diet patients are on, if they are at a reintroduction stage, they may be able to consume foods from one or more of the groups below without problems and the diet will be less restrictive. Each patient following this diet should be treated individually, so close liaison with a dietitian trained in low FODMAP diets and the catering department will be required. Foods to avoid when following a full low FODMAP diet include: Oligosaccharides (fructans, galacto-oligosaccharides) Wheat, barley, rye, onion, leek, white part of spring onion, garlic, shallots, artichokes, beetroot, fennel, peas, chicory, pistachio, cashews, legumes, lentils and chickpeas Disaccharides (lactose) Milk, custard, ice cream and yoghurt Monosaccharides (fructose) Apples, pears, mangoes, cherries, watermelon, asparagus, sugar snap peas, honey and high fructose corn syrup Polyols (sorbitol, mannitol, maltitol, xylitol) Apples, pears, apricots, cherries, nectarines, peaches, plums, watermelon, mushrooms, cauliflower and sugar free chewing gum/ mints/sweets |
|
Source |
We are grateful to Adele Thompson, Gastroenterology Dietitian for her contribution to this section. |
3.6.2 Catering for immunosuppressed patients (previously neutropenic diet)
|
Diet |
Safer Eating with Neutropenia |
|---|---|
|
Patient Groups Suitability |
Some patients who have supressed immune systems are recommended to follow food safety advice. These patients may include:
|
|
Rationale for Diet |
Following food safety advice is the new recommendation for patients that have been previously advised to follow a neutropenic, clean or low microbial diet. It is used for patients who are immunosuppressed and therefore at an increased risk of infection. Dietary restrictions are recommended to reduce the risk of infection, but nutrition must not be compromised. |
|
Menu Planning Guidance |
These patient groups are frequently in-patients for prolonged periods and may have regular readmissions for treatment, so menu fatigue can occur. Where possible these patients should be offered the widest choice with a variety of menus and food service styles to combat menu fatigue and altered taste perception. General Food Safety Advice Care needs to be taken to protect all patients from pathogenic bacteria and the risk of food poisoning. All healthcare caters should have up to date local Hazard Analysis Critical Control Point (HACCP) protocols and follow general food safety advice, including (28):
Some hospitals may allow microwave-cooked meals for patients if the HACCP protocols (see Chapter 5 for further HACCP information) are followed, core temperature has been carefully checked and noted, and they are cooked strictly to manufacturer’s guidelines. Check with your hospital for their policy regarding foods brought in by visitors. Food safety advice for neutropenic patients Please see Table 12.9 below for more specific food safety advice for neutropenic patients, i.e. patients with a neutrophil count of <1.0 (29). |
|
Source
|
We are grateful to the Haematology subgroup of the BDA Oncology Specialist Group for their original contribution to this section and Natasha Jones, Chairperson of the Haematology Sub Group for her contribution to the revision of this section. |
Table 12.9 Food safety advice for neutropenic patients (<neutrophils of <1.0)
|
Foods you can eat |
Foods to avoid |
|---|---|
|
Cheese, milk and other dairy products
|
Cheese, milk and other dairy products
|
|
Eggs
|
Eggs
|
|
Vegetables / Fruit
|
Vegetables / Fruit
|
|
Fish
|
Fish
|
|
Meat and poultry
|
Meat and poultry
|
|
Other
|
Other
|
3.6.3 Liver Disease (decompensated)
|
Diet |
Liver |
|---|---|
|
Patient Groups Suitability
|
Patients with decompensated liver disease |
|
Rationale for Diet |
Malnutrition is extremely common in people with liver disease occurring in up to 60% of those with advanced disease (30). The need to meet higher energy and protein requirements is paramount and fat or protein restriction is no longer advocated in most situations. Where these are required, a dietitian can use healthier eating choices from the menu or advise the patient on the number of protein portions per day from the standard menu. |
|
Menu Planning Guidance |
All menus should provide the opportunity for patients with liver disease to meet their energy and protein requirements (1.2 – 1.5g protein/kg body weight/day), including:
Please note: sodium restriction may be required for some patients. This should not be restricted lower than 80mmol sodium per day (1840mg sodium or 4.6g salt) and higher energy and protein requirements should still be met. A renal diet may also be required for patients with liver and renal disease. |
|
Source |
We are grateful to Julie Leaper and Susie Hamlin (Clinical Liver Leads for the BDA Gastroenterology Specialist Group) for their original contribution to this section and Dianne Wild for her contribution to the revision of this section. |
3.6.4 Test or investigation
|
Diet |
Test or Investigation |
|---|---|
|
Patient Groups Suitability |
Patients who need a medical assessment or treatment that requires dietary manipulation, including:
|
|
Rationale for Diet |
Some diets are temporary and are not necessarily nutritionally adequate. They are usually required for a test or investigation and are not suitable long term. A diet low in fibre reduces the residue left after digestion and slows the rate at which food moves through the bowel which can help to reduce common GI symptoms such as diarrhoea, bloating, wind and urgency. The term low residue is often used interchangeably with low fibre. Some pre-surgery preparation or post-surgery recovery may require patients to follow a ‘fluid only’, ‘clear fluid’ or ‘free fluid’ diet (32). |
|
Menu Planning Guidance |
General information about what low fibre diets and fluid only diets contain can vary. Therefore, local guidance should be used for these diets. The effect of fibre is individual for each patient with varying tolerance levels. There are also no technical ‘cut-offs’ for low fibre diets, however foods that are higher in fibre should be reduced or avoided if a patient requires a low fibre diet. These include:
|
|
Source |
Food Services Specialist Group (FSSG) |

