It is common to find it difficult to swallow or chew after critical illness, but it can vary between people how much it affects eating and drinking. These problems are called dysphagia.
Problems swallowing or chewing might make it difficult to eat and drink what you need to help your recovery. It can also feel frightening or worrying and make you feel like you don’t want to eat too often.
These problems usually get better as you get stronger, but if you have problems with coughing or any feelings of choking, ask your doctor or nurse to get a speech and language therapist to see you for advice.
Why does this happen?
If you have been on a ventilator (breathing machine), you may have needed a breathing tube down your throat. This can cause swelling or weakness of your throat muscles and tissues and this affects how it feels when you have food or drink in your throat. Some of the medicines you have had can also make swallowing more difficult.
How can this affect my eating and drinking?
If you had problems with swallowing or you were not able to eat when you were in hospital, you may have been fed through a tube. These feeding tubes go through your nose and then either into your stomach or into your small bowel. If you needed feeding help for some time, you may have a different type of tube that you can keep in for a longer time.
When you are able to start eating and drinking again, a Speech and Language therapist will test how easy you find it to swallow. They will advise on what foods and drinks you would find easiest to swallow safely. They may also give some exercises to help strengthen your muscles for swallowing.
How can foods and drinks be made easier to swallow?
When we drink, we first have to hold it in our mouth, then we move it to the back of our mouth, and then we swallow it. We need different muscles in our mouth and neck to do this, and when our muscles are weak, it can be difficult to do these different steps. If this is case, then it can help to choose food or drink that makes it easier to swallow.
You may find that foods or fluids with a certain ‘mouth feel’ makes them easier to chew or swallow. This is called the texture (like how thick it is or runny it is) and you may have had specific advice from the speech and language therapist about this.
You might find that foods or drinks are easier to eat if they are smooth such as pureed, soft or moist foods as these are easier to move round your mouth. These are also easier to eat if you are weak or tired, or if you find it hard to cut or chew foods. Having softer foods or foods with plenty of sauce can also make them easier to swallow. Always follow the advice from the speech and language therapist or ask to be referred if you are having difficulties with swallowing.
Thicker fluids can be easier to hold in your mouth and swallow (as thin fluids move quickly and may make you cough). Some fluids are naturally thicker (such as thick soups, smoothies or tomato juice), or you may have been advised to thicken your drinks (using a thickening powder) by your speech and language therapist. If you are having difficulties with fluids making you cough, ask to be referred to a speech and language therapist.
It can feel difficult to get used to eating different textures of food and if you are finding it difficult to swallow, you might feel like not drinking as much. But it is very important that you try to still have 6-8 cups of fluids per day to stay well. This will help your body and your recovery. You could try:
- having a little to drink more often.
- experiment with different flavours, as you might like stronger or sweeter flavours with thicker textures.
- different temperatures (hot or cold) to see if that makes it easier for you.
It’s important that you follow the advice you received from the doctor, speech and language therapist or dietitian and that you ask for help if you are unsure or finding it difficult to do.
The picture below shows different textures of food and drink. The thickness is described on a scale from zero to seven. Fluid is 0 (as it is thin) and it goes to level 4 which is very thick. Foods can be from liquidised (level 3) to an easy to chew texture (level 7). This way of describing these textures has been agreed internationally to help everyone understand it correctly for patients.
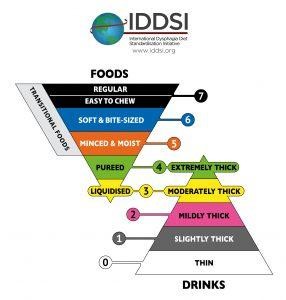
http://iddsi.org/framework/.
The IDDSI Framework and Descriptors are licensed under the CreativeCommons Attribution Sharealike 4.0 Licence https://creativecommons.org/licences/by-sa/4.0/legalcode.
As you start finding it easier to swallow and chew, you will be advised to start choosing foods that need more chewing to start moving towards eating normal food again or drinks that are a bit thinner. Your speech and language therapist or dietitian will have information for you about good meals, snack and fluid choices.
What else might the Speech and Language therapist tell me?
Your speech and language therapist may advise you on ways that you can hold your head or chin when you swallow which could help you control foods or fluids in your mouth better. They can also advise you on exercises you could do to build the strength of your swallowing muscles.
If you are worried about your swallowing or you feel like you might choke, ask your doctor to refer you to a speech and language therapist for advice.
Summary:
Swallowing difficulties should improve in time but adjusting your foods and fluids as advised by your speech and language therapist will help you continue to take enough nutrition in for your recovery.
More information:
NHS UK Advice on:
See ICUsteps information for more information