More dietitians should become supplementary prescribers, says Sharon Huish. She shares her tips on completing a non-medical prescribing course alongside a busy work life.
For a while, I had been hoping to undertake the non-medical prescribing course ‘one day’. I was led to believe independent prescribing rights for dietitians were just around the corner and had been holding out for this. However, further discussion about independent prescribing made me aware of the necessity for greater evidence, to demonstrate the demand, and need, for dietitians to work as nonmedical prescribers.
To help provide this evidence, more dietitians need to become supplementary prescribers – discovering this was the push I needed! I hope that in sharing my experience here, along with some tips and advice, I can encourage others to undertake the qualification; it’s honestly totally do-able!
Starting the course
I undertook non-medical prescribing at MSc level with the University of West England (UWE). This was a fully online course – there is considerable variation between courses delivered by different universities.
On day one we were presented with all the course submission requirements (everything we needed to do over the six months). This included:
- Initial supervision meeting, SWOT (strengths, weaknesses, opportunities, threats) analysis and action plan
- Two assignments
- A paediatric clinic visit and presentation
- Time in a pharmacy
- Two physical assessment activities (requiring sign-off)
- Two prescribing consultation activities
- Two pharmacokinetics and pharmacodynamics activities
- A mid-way review
- 90 hours of supervised learning
- And a few other activities!
I felt like I went into the course with my eyes open but I still found this first day overwhelming, as did most people. I quickly decided that information overload was not for me... I can only focus on one thing at a time, so this was the approach I took.
Initial supervision (planning) meeting
The initial supervision meeting was really helpful. My supervisors and I looked through the competencies that needed to be met and identified which competencies I would need to create opportunities for (for example antimicrobial resistance is not part of my day-to-day prescribing conversations so we identified that I could attend the ward multidisciplinary (MDT) meeting involving microbiologists).
Following this meeting, I had an action plan and I promptly booked things into my diary (the pharmacy visit, paediatric clinic shadowing, ward MDT). Top tip: from the very start, plan for how you are going to meet the competencies and get the trickier things booked in first.
The 90 supervised hours
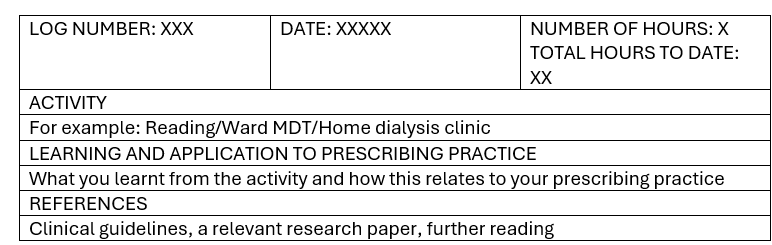
The 90 hours did not require 90 hours with my supervisors; some of the hours were with others (ward rounds, meetings or clinics) and some of the hours were reading or completing activities (for example the pharmacy visit). The 90 hours is recorded as a portfolio log, which the supervisors sign off. I laid each log entry out as below:
When I first started completing log entries I was writing far too much and each entry took me hours. After discussion with the course lead, I realised this level of detail was not required. Each log simply needed to state what the activity was and most importantly what the learning was (what I had learnt and how I could use this in practice).
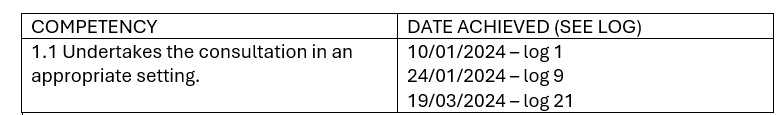
There were 76 competencies and these needed to be cross-referenced to the portfolio log (see below example). My university suggested having at least two log entries per competency (I had multiple entries for some competencies and only two for others).
There are certain things I was required to do (and document) within the 90 hours, for example a number of prescribing conversations, a pharmacy visit etc. I work four days clinically including clinics, ward work and MDT meetings; achieving the hours was no problem at all (and actually required minimal planning). I imagine more planning would be required if someone worked fewer days.
The mid-way review
This half-way review meeting was really helpful. By this point, the requirement was to have completed 40 hours of supervision. Without consciously trying, I had managed to get to 64 hours completed (although I did have to frantically complete detail within my log entries, and cross-reference the competencies, before sending it to my supervisors).
During the mid-way review, my supervisors and I identified which competencies I hadn’t met and planned for how I could achieve them. Helpfully, one supervisor also identified competencies that I had actually met but hadn’t realised. This meeting allowed me to focus the activities I did (and documented) going forward to ensure all competencies were met at the 90-hour point.
I know of others who have had 90 hours of portfolio logged without meeting all competencies and have ended up needing to do more hours!
The assignments
I was fortunate to have experience of recent academic writing – this really helped. I noticed some people got quite overwhelmed by the assignments and spent a lot of time on them, which was completely understandable.
Tips:
- Get some writing advice and support before you start (don’t let yourself get bogged down)
- Get experience of systems/functions
- Use a reference management system from the start – it will save lots of time and experience of using this will likely help you in the future
- If needing flowcharts – use SmartArt in Word
- Find out how to include landscape and portrait pages within the same document
- Make your assignment relate to your area of work/ prescribing – think of the story (protocol, debate, etc) you want to tell and then find the literature to support it (the evidence for and against)
- You don’t need hundreds of research papers – if you’re unsure, get guidance from more experienced peers or librarians on what research papers to include (for example what trials or systematic reviews)
- The key is to demonstrate your understanding of the strength of evidence as well as the limitations. For example, findings from a trial carried out in another country may have limitations for applicability in the UK if the population have differing characteristics (or if there are other differing health or social care factors)
- Demonstrate that you know the key trials underpinning the clinical guidelines, or that
- you are aware the guidelines are based on low-level evidence
The OSCE
I was petrified about the OSCE – it just felt so uncomfortable and I was full of fear beforehand. I practised with other students and also with colleagues who had previously undertaken the course, and I also memorised the history-taking proforma, which I found was a huge help.
On the day, the OSCE was better than I’d envisaged (phew!) I realised the exam was not designed to catch me out – the university had prepared us well and the practice definitely paid off. I need not have been so worried!
The written exam
The written exam was also not as bad as I had feared. We were allowed to use the BNF (British National Formulary) and also EMC (Electronic Medicines Compendium) during the exam – this demonstrates that you know where, and how, to look up the information and that you can accurately interpret it.
Tip: do the mock exams – we had two mock exams and I did each one twice. Certain topics are always covered – just a different variation. I found the mock exams helped me to identify the areas I needed to revise more. On the exam day, I found I had completed the exam with 45 minutes to spare. I spent this time re-reading the questions and my answers – I would encourage everyone to do this.
The WhatsApp group
I did not join the WhatsApp group but I know others did and found it helpful. My reason for not joining is that I did not want to know if others had finished an assignment (before I had even started) – I was working to my own timeframe and decided to block out what others were doing and when. Everyone is different.
Take-home message
I really enjoyed the non-medical prescribing course. It was full-on and a lot of work but all completely manageable despite a busy life. I have been working as a dietitian for 14 years. The years of experience (prior knowledge of medications and conditions as well as confidence in my role) really helped me during the course. The University of Surrey has developed a ‘Preparing to Prescribe’ toolkit, which is fantastic and I would highly recommend using this before you apply to undertake nonmedical prescribing.
If you are embarking on the course, the key is to identify early on (and again at the mid way review) what opportunities and support you need (to meet the competencies and complete the assignments and exams) and to create an action plan for this. If you are at a career stage where becoming a prescriber is right for you and your role, then all I can say is ‘do it’ – our profession needs you to!







