Introduction
Flowsheet of best practice recommendations
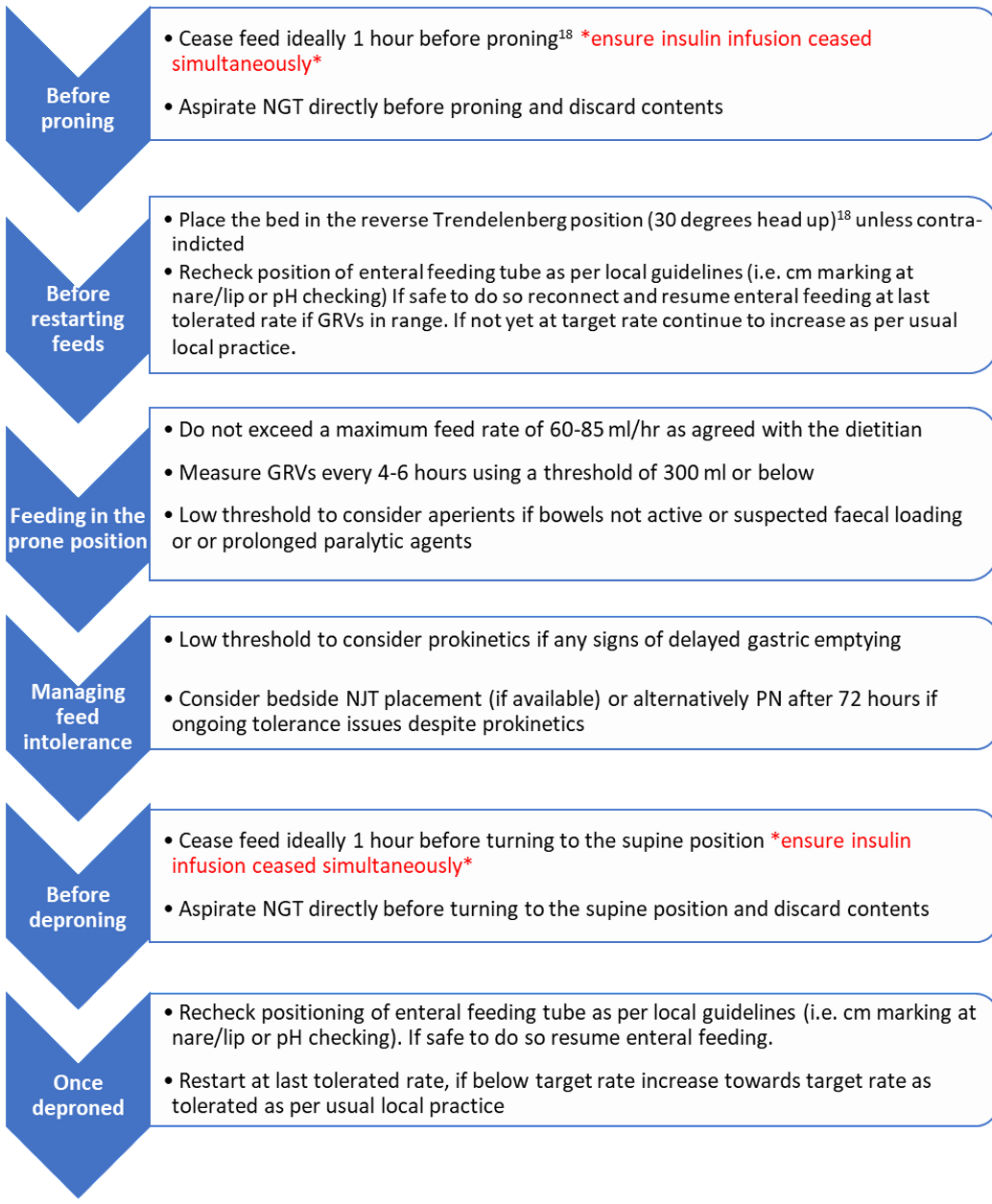
Best practice recommendations
Enteral Feeding in the intubated patient
1. Tube position
- As first line practice, consider use of a 12 French naso-gastric tube (NGT) for feeding.
- NGT insertion should only occur when the patient is in the supine position.
- If established local practice is for Naso-jejunal tube (NJT) feeding for patients in the prone position this can continue if it is practical to do so.
- NJT insertion should only occur when the patient is the supine position.
2. Feed Delivery
- Continuous enteral feeding via a feeding pump is considered best practice.
- Evidence suggests it is safe to feed at a maximum rate of 65-85mls/hr; we do not recommend higher than this whilst in the prone position.
- Gravity feeding should be avoided.
- Bolus feeding, and the use of bolused protein supplements, should not be attempted in patients whilst they are in the prone position. They should only be given when the patient is in the supine position.
3. Choice of feed
- In the first instance, a 1.3-1.5kcal/ml feed should be utilised. This should facilitate the balance between optimal feed tolerance and fluid management.
- Where strict fluid restrictions are in place, a 1.5-2kcal/ml feed may be considered with extra care given to the vigilant monitoring of gastric tolerance.
4. Monitoring feed tolerance
- In combination with other measures of gastric tolerance (i.e., bowels, abdominal distention, vomiting), NGTs should be aspirated every 4-6 hours to check GRVs.
- It is recommended that in all patients who are in the prone position, a maximum GRV of 300 ml should be used unless a lower GRV threshold is already established practice.
- It is recommended that up to 250 ml of GRVs are returned to the patient and the remainder are discarded, unless a more conservative practice is already established locally.
5. Managing Feed Intolerance
- If a GRV exceeds the threshold at any time, commencing prokinetics in accordance with local guidelines is recommended. If gastric aspirates remain above the threshold after 12-24 hours of prokinetic use, a second line of feeding should be considered:
- If further sessions in the prone position are anticipated over the next 48 hours or more, consider bedside placement of NJT when patient is in the supine position.
- If the NJT does not have a gastric port, it is recommended that an NGT is inserted for free drainage.
- If NJT placement is not possible or feed tolerance has not improved, parenteral nutrition (PN) should be considered.
- Upon initiating PN, where possible, concurrent trophic enteral feeding should be considered.
Oral nutrition in awake patient in the prone position (including on non-invasive ventilation (NIV/CPAP/HFNO)
- This group of patients are at high risk of aspiration. Swallow safety should be monitored and where indicated, referral to a Speech and Language therapist should be made.
- Oral diet should be encouraged, if safe to swallow, once the patient is out of the prone position and when off non-invasive ventilation (NIV) or CPAP.
- Patients receiving high-flow nasal oxygen (HFNO) in the supine and sitting position, may achieve a reduced oral nutritional intake.
- The use of oral nutrition supplements is recommended to optimise nutritional intake, particularly if the patient has missed meals/snacks due to time spent in the prone position.
- Consider NGT insertion for nutrition, if the patient is on HFNO and their oral intake is <50% of energy requirements for more than five days
- For those on NIV, it is recommended that an NGT is inserted for nutrition.
Enteral feeding in the awake, patient in the prone position (including on non-invasive ventilation (NIV/CPAP/ HFNO)
Follow recommendations as above in the ‘enteral feeding in the intubated patient’ section, with the additional considerations:
1. Reducing aspiration risk
- Consider early or prophylactic prokinetics and proton pump inhibitors, particularly for those with pre-admission history of oesophageal regurgitation or reflux regardless of GRV.
- Regularly ask patients if they experience any reflux, fullness, nausea or vomiting. This would be an indication to temporarily stop enteral feeding.
- Monitor closely for signs of gastro-intestinal intolerance in patients on NIV (or who may have prolonged periods of coughing or mouth breathing); as this can lead to excessive swallowing of air and gastric distension.
2. Maximising feed delivery
- If the patient is having frequent position changes (i.e., ½ hour – 2 hourly) avoid prolonged and premature cessation of NGT feeding. Aspiration of stomach contents prior to the position changes can help reduce this. Follow guidance above on GRV management.
- Prior to planned intubation, the aspiration of stomach contents can be undertaken; with NGT feeding continuing up to 2 hours pre-intubation if ICU team agree.
- With the patient’s consent, consider the use of a nasal bridle feeding tube retaining device to reduce the risk of tube misplacement during turning into and out of the prone position.
- If there are significant interruptions to enteral feed delivery, consider use of a modified ‘catch-up regimen’ when the patient is in the supine position using a target volume of feed required per 24 hours.
- Catch up regimens should not exceed a maximum rate of 65-85mls/hr and the use of higher kcal/ml feeds may be required. This approach should be used with caution and is only recommended for those units familiar with the practice.
3. Additional positioning considerations
- If lying flat-bed, face-down in the prone position i.e., NOT in reverse Trendelenberg position, stop NGT feeding during this time as aspiration risk is higher.
- If the patient is deemed at nutritional risk and has not received nutrition for greater than 72 hours, discuss with the ICU team options for bedside NJT placement or PN.
- As long as it is tolerated, NGT feeding should continue when the patient is lying on their right and left sides with the bed flat.
Published Studies Used to Inform Recommendations
Six studies were identified investigating enteral feeding in the prone postion4-9. All were small in sample size and based primarily on observational study designs. The quality of the available evidence is therefore low and should be interpreted with these limitations in mind. Three international guidelines on nutrition in COVID-19 were identified10-12 and five review articles which provided clinical insights13-17.
Route of Delivery
All international guidelines for nutrition in COVID-19 support the use of EN whilst in the prone position and advocate the use of post pyloric tubes if tolerance is an issue10-13. Due to the aerosol generating risks associated with post pyloric tube placement endoscopically or via interventional radiology, a case-by-case decision is recommended. No difference in micro-aspiration was observed between gastric and post-pyloric tube feeding in patients undergoing rotational positioning for ARDS5. All other studies in the prone position used gastric feeding tubes, and no increased incidence of ventilator associated pneumonia was observed in comparison with those in the supine position4;6.
Gastric Residual Volumes
No published studies were identified comparing the risk of aspiration based on different GRV thresholds whilst in the prone position. Most commonly a GRV of 250mls has been used whilst feeding in the prone position4;6,9.
Enteral Feeding Regimens
All international guidelines for nutrition in COVID-1910-12 advocate for continuous enteral feeding using pumps with an incremental increase in rate over the first 4-7 days to avoid gastro-intestinal complications and risks associated with overfeeding. The safe maximum feeding rate whilst in the prone position has been suggested to be between 65 ml/hr4 to 85 ml/hr6.
Reducing gastrointestinal complications
Episodes of vomiting and aspiration have been witnessed particularly when turning the patients from supine to prone position and vice versa15. Cessation of NG feeding for 1hr prior to position change has been suggested as a way of overcoming complications11;15;18.
Oral intake in self-ventilated patients, on NIV in the prone position
Patients in the supine position on HFNO or NIV experience difficulties in meeting their nutritional requirements orally10. It can therefore be assumed that the prone position will further amplify this problem. Due to the lack of evidence to support decision making, an individualised approach to feeding whilst receiving NIV support in the prone position is required, taking into account nutritional risk, oral intake, resources and degree of respiratory compromise10.
References and Disclaimer
Disclaimer:
The CCSG writing group have written these guidelines based on the evidence available and clinical experience. We acknowledge that enteral nutrition of those in the prone position, especially whilst on NIV, is not without risk. We recommend all feeding decisions are made in agreement with the local critical care team, including a local risk assessment.
References
- Sud S, Friedrich JO, Adhikari NK, Taccone P, Mancebo J, Polli F, Latini R, Pesenti A, Curley MA, Fernandez R, Chan MC. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. CMAJ. 2014 Jul 8;186(10):E381-90.
- Meng L, Qiu H, Wan L, et al.Intubation and Ventilation amid the COVID-19 Outbreak. Anesthesiology. 2020;Publish Ahead of Print. doi: 10.1097/ALN.0000000000003296. Accessed March 29 2020.
- Bamford P, Bentley A, Dean J, Whitmore D, Wilson-Baig N. ICS Guidance for Prone Positioning of the Conscious COIVD Patient 2020. Intensive Care Society. https://www.ics.ac.uk/ICS/COVID-19/COVID-19/COVID-19_Home.aspx?hkey=d176e2cf-d3ba-4bc7-8435-49bc618c345a
- Reignier J, Thenoz-Jost N, Fiancette M, Legendre E, Lebert C, Bontemps F, Clementi E, Martin-Lefevre L. Early enteral nutrition in mechanically ventilated patients in the prone position. Critical care medicine. 2004;32(1):94-9. doi: 10.1097/01.CCM.0000104208.23542.A8
- Sams VG, Lawson CM, Humphrey CL, Brantley SL, Schumacher LM, Karlstad MD, Norwood JE, Jungwirth JA, Conley CP, Kurek S, Barlow PB. Effect of rotational therapy on aspiration risk of enteral feeds. Nutrition in Clinical Practice. 2012;27(6):808-11. doi:10.1177/0884533612462897
- Reignier J, Dimet J, Martin-Lefevre L, Bontemps F, Fiancette M, Clementi E, Lebert C, Renard B. Before–after study of a standardized ICU protocol for early enteral feeding in patients turned in the prone position. Clinical Nutrition. 2010;29(2):210-6. doi:10.1016/j.clnu.2009.08.004
- van der Voort PH, Zandstra DF. Enteral feeding in the critically ill: comparison between the supine and prone positions: a prospective crossover study in mechanically ventilated patients. Crit Care. 2001;5:216. doi:org/10.1186/cc1026
- Saez de la Fuente I, Saez de la Fuente J, Quintana Estelles MD, Garcia Gigorro R, Terceros Almanza LJ, Sanchez Izquierdo JA and Montejo Gonzalez JC. Enteral Nutrition in Patients Receiving Mechanical Ventilation in a Prone Position. Journal of Parenteral and Enteral Nutrition. 2016;40:250-255. doi:10.1177/0148607114553232
- Savio RD, Parasuraman R, Lovesly D, Shankar B, Ranganathan L, Ramakrishnan N, Venkataraman R. Feasibility, tolerance and effectiveness of enteral feeding in critically ill patients in prone position. Journal of the Intensive Care Society. 2020; Published Ahead of Print. doi:10.1177/1751143719900100. Accessed March 29 2020.
- Barazzoni, R., Bischoff, S. C., Breda, J., Wickramasinghe, K., Krznaric, Z., Nitzan, D., ... & Singer, P. (2020). ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection.
- Chapple, L. A. S., Fetterplace, K., Asrani, V., Burrell, A., Cheng, A. C., Collins, P., ... & Ridley, E. J. (2020). Nutrition management for critically and acutely unwell hospitalised patients with coronavirus disease 2019 (COVID‐19) in Australia and New Zealand. Nutrition & Dietetics, 77(4), 426-436.
- Martindale, R., Patel, J. J., Taylor, B., Arabi, Y. M., Warren, M., & McClave, S. A. (2020). Nutrition Therapy in Critically Ill Patients with Coronavirus Disease (COVID‐19). Journal of Parenteral and Enteral Nutrition.
- Thibault, R., Seguin, P., Tamion, F., Pichard, C., & Singer, P. (2020). Nutrition of the COVID-19 patient in the intensive care unit (ICU): a practical guidance. Critical Care, 24(1), 1-8.
- Thibault, R., Coëffier, M., Joly, F., Bohé, J., Schneider, S. M., & Déchelotte, P. (2020). How the Covid-19 epidemic is challenging our practice in clinical nutrition—feedback from the field. European journal of clinical nutrition, 1-10.
- Arkin, N., Krishnan, K., Chang, M. G., & Bittner, E. A. (2020). Nutrition in critically ill patients with COVID-19: Challenges and special considerations. Clinical Nutrition (Edinburgh, Scotland).
- Mehta S. Nutritional Status and Covid 19: An opportunity for lasting change? COVID 19 Rapid Report Clinical Medicine. 2020 Vol 20, No 3: 270-38)
- Patel, J. J., Martindale, R. G., & McClave, S. A. (2020). Relevant Nutrition Therapy in COVID‐19 and the Constraints On Its Delivery by a Unique Disease Process. Nutrition in Clinical Practice, 35(5), 792-799.
- ICS/FICM Guideline Development Group. Guidance For: Prone Positioning in Adult Critical Care . Version 1, November 2019.