Following a coronavirus (COVID-19) infection, symptoms can last for more than 12 weeks. This is called Long Covid. Symptoms vary a lot. They affect people differently and affect many different body systems.

What is Long Covid?
Long Covid does not seem to be linked to how ill you are when you first have COVID-19. Most people can expect to get better over time.
Common reported symptoms include:
- extreme tiredness (fatigue)
- memory and concentration problems ("brain fog”)
- feeling sick, diarrhoea, stomach aches, loss of appetite
- changes to smell or taste
- shortness of breath
- chest pain or tightness, heart palpitations
- difficulty sleeping (insomnia)
- dizziness
- joint pain
- pins and needles
- depression and anxiety
- tinnitus, earaches
- high temperature, cough, headaches, sore throat
- rashes
It is important to check ongoing symptoms with your doctor, to make sure there are no other causes. Many of these symptoms can affect your ability to eat well.
What is the best diet for recovery?
Eating can be challenging when you are unwell. But your body needs a balanced and wide variety of vitamins, minerals, protein, energy, fibre and fluid to work best and help recovery. A good intake helps your muscles to rebuild, maintains your immune system and increases your energy levels.
Diets with this balance and diversity include the Mediterranean type diet (considered to be an anti-inflammatory diet) and the NHS Eatwell Guide.
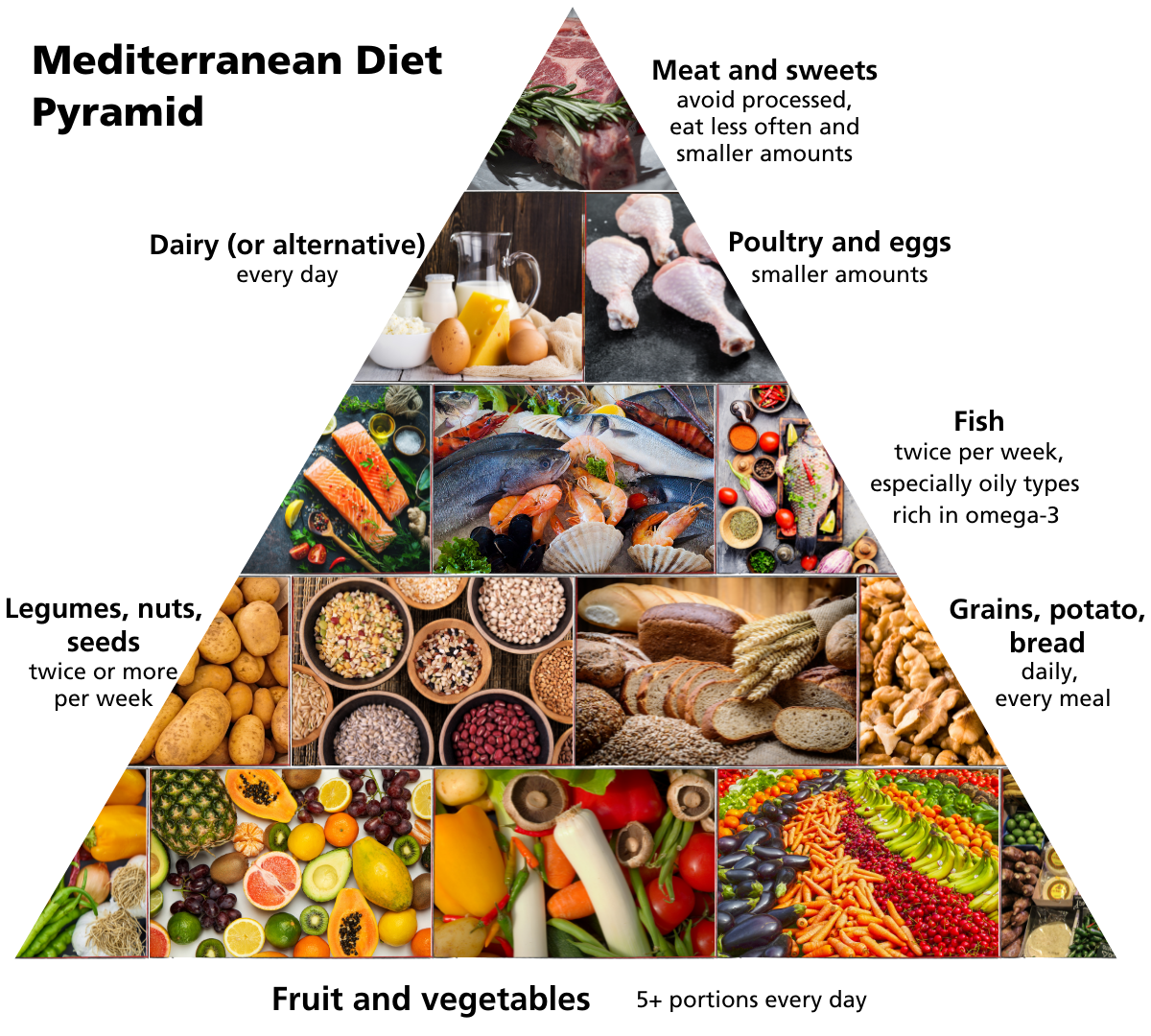
- Base your meals on potatoes, bread, rice, pasta or other starchy carbohydrates, as they are a good source of energy. Wholegrain types are good for fibre and often release energy more slowly: this is known as having a low glycaemic index and may help when struggling with fatigue
- Each day, aim to have at least five portions of a variety of fruits and vegetables, for vitamins, minerals and fibre. Fresh, frozen, tinned or dried all count
- Beans, pulses, nuts and seeds, fish, eggs and meat are good sources of protein. Eat red meat less often and small portions only, especially processed types like sausages, burgers, bacon. Find out more about plant-based alternatives to meat here
- Fish is low fat and good to include twice a week, especially oily types such as salmon, and sardines, which are rich in omega-3. Plant-based sources of omega-3 include certain nuts, seeds, oils, soya and omega-3 enriched foods - check out our Omega-3 fact sheet for more info
- Milk, cheese and yoghurt are sources of protein and some vitamins. They’re also an important source of calcium, which keeps bones healthy. If choosing dairy-free alternatives, make sure they are fortified with calcium
- Choose unsaturated oils and spreads in small amounts
- Drink plenty of fluids, especially water, milk or sugar-free drinks. Fruit juice and smoothies also count, but limit these to 150ml per day
What if I am losing weight and have a poor appetite?
Try smaller amounts more often, and include easy snacks and nourishing drinks. For more ideas see NHS Your COVID Recovery. If you continue to lose weight, ask your doctor to refer you to a dietitian, who can tailor advice to your needs and help you meet your goals. You may be prescribed nutritional drinks to help boost intake and your weight.
What might help with smell and taste changes?
Some people experience loss or change in smell and taste, following a COVID infection. These changes usually don’t last long, but can affect your eating. There are helpful tips at NHS Your COVID Recovery, and the charity AbScent. For instance, adding strong flavours such as spices, or sharp and bitter tastes like citrus may help. Some people find that varying the textures of their food keeps it interesting. Food served cold or at room temperatures are often better tolerated.
What can I do to help my gut health?
Common gut symptoms in Long Covid are feeling sick, bloating, pain and diarrhoea. These are irritable bowel syndrome (IBS) type symptoms. If these persist, speak to your doctor, as it’s important to rule out other causes like Coeliac disease. They can also refer you to a dietitian. The BDA Food Fact Sheet on IBS has useful tips to help you manage the different symptoms.
There is emerging evidence that the gut microbiome, (bacteria and small organisms in the gut), plays an important role in our health. Eating for gut health involves a varied and diverse range. Eat lots of different colours of plant-rich foods providing fibre, such as fruit, veg, nuts, seeds, beans, pulses and wholegrains.
Probiotics are also worth considering to help gut symptoms, although there is no evidence that these help Long Covid. A trial of one month only is recommended to test if it’s beneficial. Find out more in the BDA's probiotics fact sheet.
Stress, anxiety and sleep disturbance can all affect your gut health, making symptoms worse. Psychological or talking therapies can help with this.
Should I take vitamin and mineral supplements?
Vitamin D is needed for bone and muscle health, as well as immunity. A daily vitamin D supplement of 10 micrograms or 400IU is recommended for all UK adults from October to April. If you have little or no sunshine exposure because of Long Covid, and are spending most of your time indoors, you should take the supplement all year.
If you are only eating small amounts, or are unable to eat well, you risk a low intake of vitamins and minerals. You may wish to take a one-a-day A-Z multivitamin and mineral supplement, of no more than 100% recommended intake.
Some people with Long Covid believe that high doses of vitamins, such as niacin (vitamin B3), vitamin C, vitamin D, quercetin and zinc improve their symptoms. However, there is no scientific evidence that these supplements work, and taking high doses can harm you. It is best to take a one-a-day multivitamin and mineral supplement, rather than large doses of individual vitamins or minerals.
What about a low histamine diet and Long Covid?
It has been suggested that some people with Long Covid may become sensitive to histamine in food. This may be either because the body’s histamine levels rise during inflammation or because it may struggle to break down dietary histamine. As yet there is no evidence that a low histamine diet helps most people with Long Covid.
A low histamine diet involves a two to four week trial period. Many foods high in histamine are restricted. They are then reintroduced systematically, one-by-one, to test tolerance. If you do this, we recommend support from a dietitian, to minimise nutritional risk.
This diet is time-consuming to prepare. Many have found it difficult to follow, especially with their fatigue and other debilitating symptoms. Although there are online lists of histamine content in foods, the reported levels are not consistent. Additionally, the low histamine diet goes against the principles of the Mediterranean type diet, by avoiding such foods as oily fish and some fruits and vegetables. The Mediterranean type diet is much healthier and easier to follow.
How a dietitian can help
Ask your GP or doctor to refer you to a dietitian if you are:
- Losing or gaining weight unintentionally
- Unable to eat well due to smell or taste changes, fatigue, nausea, gut symptoms, or other Long Covid symptoms
- Following a restrictive diet
Alternatively, you may wish to see a private dietitian.
Top tips
- Plan ahead, if possible, for easy, quick snacks, meals and nourishing drinks.
- Eat regularly.
- Avoid restrictive diets.
- Aim for a Mediterranean type diet, including a diverse range of plant-rich food.
- Check for any unwanted weight changes - aim to keep a steady healthy weight.
- Be kind on yourself. Eating can be difficult enough when you are unwell. Small changes often work best.
Source(s)
Long-term effects of coronavirus (long COVID) [Internet]. nhs.uk. 2022 [Accessed 23 February 22]. Available from: https://www.nhs.uk/conditions/coronavirus-covid-19/long-term-effects-of-coronavirus-long-covid
Salamanna, F et al. Front Med (Lausanne). 2021; 8: 653516. “Post-COVID-19 Syndrome: the persistent Symptoms at the Post-viral Stage of the Disease. A Systematic Review of the Current Data” Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8129035 [Accessed 23 February 22]
University of Plymouth Nutrition and COVID-19 Recovery Knowledge Hub [Internet] (https://www.plymouth.ac.uk/research/dietetics-and-health/covid-knowledge-hub ; Prof Calder Nutrition and COVID-19 Recovery: Is there an anti-inflammatory diet? Available from: https://www.youtube.com/watch?v=r7A-cONFir4 [Accessed 23rd February 22]
The Eatwell Guide [Internet]. nhs.uk Available from: https://www.nhs.uk/live-well/eat-well/the-eatwell-guide [Accessed 23 February 22]
National Institute for Health and Care Excellence (NICE)) “Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management” [NG206] Published: 29 October 2021. Available from https://www.nice.org.uk/guidance/ng206 [Accessed 23 February 22]
British Dietetic Association. Omega-3 Food Fact Sheet [Internet]. BDA.uk.com. 2019 [Accessed 23 February 2022]. Available from https://www.bda.uk.com/resource/omega-3.html
Eating Well [Internet]. Your COVID Recovery. 2022 [Accessed 23 February 2022]. Available from: https://www.yourcovidrecovery.nhs.uk/your-wellbeing/eating-well/
Taste and Smell [Internet]. Your COVID Recovery. 2022 Available from: https://www.yourcovidrecovery.nhs.uk/managing-the-effects/effects-on-your-body/taste-and-smell [Accessed 23 February 2022].
AbScent Anosmia Support [Internet] [Accessed 23 February 2022]. Available from: https://www.youtube.com/c/AbScentAnosmiaSupport
British Dietetic Association. Irritable Bowel Syndrome Food Fact Sheet [Internet]. BDA.uk.com. 2019 [Accessed 23 February 2022]. Available from: https://www.bda.uk.com/resource/irritable-bowel-syndrome-diet.html
British Dietetic Association Probiotics Food Fact Sheet [Internet] BDA.UK.com [Accessed 23 February 2022]. Available from https://www.bda.uk.com/resource/probiotics.html
National Institute for Health and Care Excellence (NICE)) " COVID-19 rapid guideline: Vitamin D” [NG187] Published: 17 December 2020 [Accessed 23 February 2022] Available from https://www.nice.org.uk/guidance/ng187
National Institute for Health and Care Excellence (NICE)) “Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management” [NG206] Published: 29 October 2021. Available from https://www.nice.org.uk/guidance/ng206 [Accessed 23rd February 22]
What to eat when you have COVID-19 or long COVID [Internet]. Published 24 August 2021. Covid.joinzoe.com. 2022 [Accessed 23 February 2022]. Available from: https://covid.joinzoe.com/post/long-covid-diet-nutrition
Vitamins and minerals [Internet]. nhs.uk. 2022 [Accessed 23 February 2022]. Available from: https://www.nhs.uk/conditions/vitamins-and-minerals
British Dietetic Association. Caution advised with Low Histamine diets for Long Covid [Internet] Published 20 May 2021 [Accessed 23 February 2022] Available from: https://www.bda.uk.com/resource/caution-advised-with-low-histamine-diets-for-long-covid.html
British Dietetic Association. Low Histamine diets and Long Covid [Internet] Published 1 April 2021 [Accessed 23 February 2022] Available from: https://www.bda.uk.com/resource/low-histamine-diets-and-long-covid.html
Skypala IJ, Williams M, Reeves L, Meyer R, Venter C. - Sensitivity to food additives, vaso-active amines and salicylates: a review of the evidence. Clin Transl Allergy. 2015 Oct 13:5:34 [Accessed 23 February 2022] Available from: https://pubmed.ncbi.nlm.nih.gov/26468368







