Introduction
Symptoms/difficulties with eating after critical illness
As mentioned in the ‘Nutrition in Hospital after Critical Illness’ information sheet, recovering from being critically ill can come with physical and emotional difficulties and these can last for some months after leaving hospital.
It can sometimes feel hard to get back to eating normally after a critical illness. There are a number of symptoms that could affect eating. Although you may not have all of these difficulties, you may have had some which are now improved, but other difficulties may last longer. You may find that your appetite is not quite back to normal or that you have a reduced interest in eating because you feel so tired or weak. When you eat, you may find that food does not taste quite as it should, you may have a dry mouth, or you may feel full quickly. Some people continue to have some difficulties with swallowing, so if eating and drinking makes you cough, please do tell your GP or dietitian. Stomach problems like feeling sick, indigestion, having upset bowels, bloating, or constipation can happen for a short time when you are home. It is important to have enough to drink and eating the right foods to help with your recovery and also help your hair, nails and skin grow well.
For further information and advice on these common difficulties or symptoms after critical illness, please see the ‘Tips to help with eating problems after Critical Illness’ information sheet.
Regaining muscle and strength during critical illness recovery
You may find that you have lost a lot of weight after being critically ill. You may now be underweight and need to put on some weight. If your weight is now in the healthy or overweight range, you may still have noticed muscle loss. Getting back some of the weight and muscle you have lost can help give you more energy and strength to slowly become more physically active again.
Physical activity is an important part of your recovery. To begin with, this activity will be simply starting to move around again. On the intensive care unit (ICU) and on the ward, physiotherapists will have helped you start using your muscles again by sitting on the edge of the bed, bed cycling or walking. As you got stronger, it would have included doing more for yourself, like making a drink or snack, washing yourself and doing simple household tasks.
Doing physical activity is part of your rehabilitation (things that will help you recover from your critical illness) and when you are feeling stronger, you can then start doing gentle exercise to continue to build your strength. This activity can be one that helps your heart and circulation (called aerobic exercises) or one that will help your muscles get stronger (strengthening exercises). The physiotherapists who helped you in hospital, will have given you advice about this. For more information look at ICUsteps information sheet ‘Helping you to recover after Critical Illness’.
As well as this activity, you will need a high protein and high energy diet to help you build muscle and get stronger.
Some people feel that although they put weight back on, getting back muscle takes much longer. If this happens for you, it may help to keep eating a high protein diet while cutting back on high fat and energy foods. See the healthy eating tab above for more tips about this.
High energy and protein diet to help recovery
The amount of energy and protein our bodies need varies from person to person, but to help with recovery after critical illness, you will probably need to eat more than you did before. This is because you may need to put on weight, or get back some muscle, or need to have energy for your muscles to help build strength to be more active. You may also find that you still do not eat as well as you used to (either because you do not feel very hungry or just not being very interested in eating). Your doctor or dietitian may have advised you to have a diet high in protein and energy to help your recovery, so please do follow their advice as this will be the right advice for you.
To start with, here are some tips to help you eat:
- be positive about what you are able to eat – every extra mouthful helps
- eat whenever you feel hungry– like having cereal at midnight
- try different foods. You may find that you like things you don’t usually eat
- keep snacks nearby where you are, such as on the bedside table or coffee table
- try not to drink just before meals as this may fill you up and spoil your appetite, unless you need to drink to help with swallowing
- although salads and vegetables are an important part of a healthy diet, don’t eat too much with each meal if they are filling you up quickly
- avoid fizzy drinks as they can make you feel full up
- accept offers from friends and relatives for help with cooking and shopping
- convenience foods are a useful standby and can be just as nourishing
- when you are stronger and if you are able to cook for yourself, try to prepare food in advance when you feel like cooking and store it in the freezer (if you have one) for when you are not feeling so well
- a short walk before a meal or some fresh air may help you feel hungry.
How can I have enough protein and energy?
Sometimes after critical illness, a plate of food (such as you used to eat) can feel really overwhelming. So, to begin with, the best plan is to eat ‘little and often’, try to eat smaller portions more often by including snacks between meals and before bed so you eat every 2-3 hours (so eating 6 times a day). As you become used to eating again, you will gradually build up how much you are able to eat at each meal.
Here are some high protein and energy snack ideas:
|
fruit with cream/custard |
creamy yogurt |
crème caramel |
|
custard tart |
custard pot |
rice pudding |
|
trifle |
mousse |
cheesecakes |
|
biscuits |
cakes |
mini chocolate/cereal bars |
|
nuts |
cheese/pâté and crackers |
cheese cubes |
|
crisps |
savoury biscuits |
bread sticks with humus/dips |
|
olives |
sandwiches |
salmon rolls |
|
small pieces of pizza |
flan |
pork pies |
|
pasties |
scotch eggs |
sausage rolls |
|
pakoras |
Bombay mix |
halva |
|
bhajis |
spring rolls |
crumpets |
|
bagels |
muffins |
scones |
|
croissants |
toast |
breakfast cereal |
If you are only eating small amounts of food and you need to put on more weight, choose full fat foods instead of “light” or “diet” versions, as these are not right for you at the moment if you need to have more energy. If you have diabetes or high blood cholesterol, please ask your doctor or dietitian for advice on foods high in energy or protein that are suitable for you to eat.
You can also fortify your foods and drinks to get more energy and protein without having to eat more food. Fortifying means adding something to it, to give it more energy or protein. The following section gives you some tips on how to do this.
Tips for adding extra energy and protein (fortifying) your foods and drinks
There are many ways to add extra energy and protein to your food, for example:
Milk can be fortified by adding 2oz (4 tablespoons) of milk powder (such as Marvel or supermarket own brand) to 1 pint of full cream milk. Adding milk powder gives extra protein and more energy. This fortified milk can then be used in the usual way in drinks, on cereals, in sauces and puddings.
Savoury foods can be fortified, for example:
- add beans, pulses or ground nuts (like almonds), seeds, soy protein powder, pea protein powder, chick pea flour, or gram flour to soups and casseroles
- add nut butters (like peanut butter, almond butter, or cashew butter) to soups, casseroles or sauces over meals
- add cheese, milk, milk powder, butter, margarine or olive oil into mashed potato
- add 2 tablespoons of milk powder to a portion of white or cheese sauce
- add butter, full-fat margarine, cheese or white sauce on vegetables
- add cheese/cream/milk or crème fraîche to soup
- add cream/sour cream/crème fraîche or coconut milk to casseroles and curries
- add mayonnaise/salad cream or pesto to sandwiches or have two fillings, such as: egg mayonnaise and bacon or cheese and ham.
Fortify sweet foods, for example:
- add 2 tablespoons of milk powder to a portion of porridge, milk puddings and custard
- add nut butters (like peanut butter, or almond butter, or cashew butter) to puddings
- add cream, custard, condensed milk, evaporated milk, fortified milk, or ice cream to pies, sponge or fruit
- add extra sugar, honey or syrup to desserts and cereals make jelly with fortified milk, instead of water
- add cream, yoghurt, sugar, honey, condensed/evaporated milk or dried fruit to breakfast cereals.
If you have diabetes or high blood cholesterol, please ask your doctor or dietitian for advice on foods high in energy or protein that are suitable for you to eat.
Tips for increasing your protein intake:
The long-term after effects of critical illness often include a loss of muscle protein and difficulty in regaining some muscle mass and strength. Eating enough protein along with doing physical activity will help this.
Your body uses protein to build and repair tissues. Protein is an important building block of bones, muscles, cartilage, skin, hair, nails and blood. Both energy and protein are important building blocks which help our bodies recover, repair and regain our strength.
This section gives tips about how to eat more protein.
You should try to have high protein foods at each meal, and have a milky dessert between your meals. If you have a kidney disease, please ask your doctor or dietitian for advice on protein intake.
The following foods are good sources of protein:
- Meat: eating meat or poultry (such as chicken) and slightly larger portions (if you are able to) is an easy way to increase your protein intake. Try to choose cuts of meat without too much fat on them. If you find it difficult to chew and swallow meat, try cutting it into small pieces, or having it with gravy or sauce so it’s not too dry.
- Pulses: (for example lentils or beans) are high in fibre and a source of iron, as well as being affordable. If you buy tinned pulses, check the label and choose ones that have no added salt or sugar. They are easy add-ins to sauces, soups and stews, even if they’re not used in the original recipe.
- Soya: are high in good quality protein, low in fat and contain fibre and iron. Examples are a glass of soya milk, a pot of soya yoghurt or tofu.
- Quinoa: is a good protein food and an easy substitute for rice and pasta.
- Nuts: provide protein and are packed with fibre. Although they are high in fat (and so are high in energy), most of this fat is heart-healthy unsaturated fats. Choose nuts which have not had salt added to them.
- Seeds: (such as sunflower or pumpkin seeds) contain healthy unsaturated fats and protein. They can be easily added to salads and pasta, or you can eat them plain as a simple snack.
- Cereal and grains: wholegrain (called wholemeal or brown) breads, rice and pasta have more protein, fibre and iron than white versions.
- Quorn/Mycoprotein & other Textured vegetable protein alternatives: these have a meat-like texture and are low in saturated fat. They are sold in a range of forms from mince, pieces, nuggets, sausages and fillets, so they can easily be swapped with meat.
- Milk & Dairy products: milk, yoghurt and cheese are great sources of protein and also contain calcium to keep our bones healthy. Dairy alternatives are much lower in protein but fortified versions are still a very good sources of calcium.
- Eggs: are low in saturated fat and good sources of vitamin B12 and vitamin D. Generally there is no limit to how many eggs you can eat, but there are some medical conditions (such as familial hypercholesterolemia) which means you may need to not eat too many, so ask your doctor or dietitian for advice.
- Fish & Seafood: white fish is a low-fat protein source. Oily fish, such as sardines, mackerel or salmon, are a little higher in fat but contain omega-3 fatty acids, which are heart healthy and contain vitamins A&D. Seafood includes prawns, crab, lobster, mussels, oysters, scallops and clams. These can be brought fresh, frozen and in tins.
The table below gives you an idea of the approximate amount of protein per serving size. Even if you do not need to work out how much protein you have, it may be a helpful guide to help you have more protein.
|
Food Group |
Item and serving size |
Amount of protein (g) |
|
Breads and cereals |
2 slices bread ½ cup rice or pasta ¾ cup breakfast cereal 2 plain biscuits |
6 2 2 2 |
|
Starchy vegetables |
1 medium potato |
3 |
|
Meat and fish |
150 g, raw, lean red meat 150 g raw chicken breast 150 g raw fish 1 can tuna 2 eggs |
33 33 25-30 25 12 |
|
Dairy |
250 ml milk 250 ml almond milk 200g Greek yoghurt 35 g cheese |
8 1 10-20 9 |
|
Beans and legumes |
100 g Tofu 30 g nuts ½ cup legumes |
10 5-7 7 |
How can I have extra energy from drinks?
You can choose to have drinks that can give you extra nutrition. For example:
- Hot drinks: hot chocolate, Ovaltine/malted drinks, milky coffee, latte, cappuccino, instant soups made with fortified milk
- Cold drinks: milkshakes with added ice cream/cream, fruit smoothie (blended fruit with milk), ice cream/yoghurt with honey/malt, ice cream soda (ice cream added to a fizzy drink), fruit juice.
You can also have special drinks that are high calorie and protein drinks (also called nutritional supplement drinks). You may have had these recommended from your hospital stay and advised to continue them until you reach a better weight, or you are eating full meals. If you are uncertain about how to take them, or how long for, please contact your doctor or dietitian for advice.
Nutritional supplement drinks come in a wide range of different types and flavours for example:
- Nourishing powdered drinks: Complan and Meritene are common brands. These are available from most chemists/supermarkets and are often advised as the first type to try before moving onto the ready-made ones below. They can also be added to foods to increase their nutrient content
- Nutritional supplement drinks: come in milkshake, juice or jelly styles. They also come in a variety of sizes, for example, there are compact types that give the same nutrition but in a smaller volume. You may have had these in hospital, and may have been told to continue them. They can be provided on prescription from your GP, but may have a different name (be a different brand) than those in hospital. Check with your pharmacist that they are similar (for example in protein content). If you are unsure about having these drinks, or you are not having them, but think they may help you while you are struggling with your eating or weight, speak to your dietitian or your doctor for advice.
Healthy eating in the later stages of recovery
In the months or years after critical illness, you might feel like you are putting on more weight than you need, but you are not gaining enough muscle. At this point, you may want to start choosing a healthy diet, having less fat and energy. This will help you either keep your weight steady, or help you to lose a little weight if this is best for your long-term health.
Below is some information about eating a healthy, balanced diet and at the bottom there are more tips if you want to lose weight.
How can I eat a balanced diet?
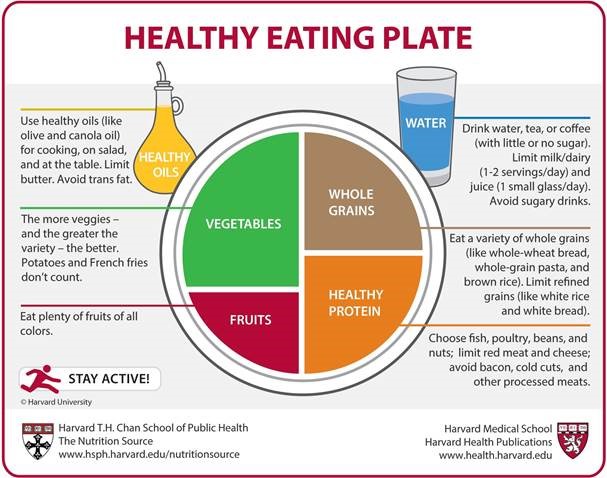
A balanced diet is about having the right types and amount of foods that are good for you. One way to do this is to use the Eatwell Guide from Public Health England (see the link in the More information section). This explains the different food groups that should be part of a healthy balanced diet, including fruit and vegetables, protein, carbohydrates and dairy (or dairy alternatives). You need to try and eat some of these foods most days, and the picture gives an idea of how much to eat. You do not have to get this balance in every meal but roughly over a week.
It is helpful to make every meal as balanced as possible, and the Harvard Healthy Eating Plate picture (below) gives you an idea on how to do this. The Harvard Eatwell plate is a good visual guide for portion sizes on a plate. The advice to limit milk and dairy is not advice supported by the British Dietetic Association Try to make sure that half of your plate is filled with vegetables, salad, fruit or a mixture of them. The other half can be equally divided between starchy foods (such as pasta and bread), and foods high in protein (such as meats, dairy, eggs and nuts). It is particularly important to have enough healthy choices of protein during recovery as our bodies use this to help with healing and building muscle, so make sure you try to have a quarter of the plate as protein.
What are the different types of food groups?
Fruit and Vegetables
Fruit and vegetables should make up just over a third of the food eaten.
Aim to consume at least 5 portions of a variety of fruit and vegetables every day, having different colours and types. These do not have to be just fresh, so you can also include frozen, tinned, dried and unsweetened juices and smoothies. Try to avoid adding foods high in sugar or fat to fruit and vegetables, such as butter or syrups. To help eat more fruit and vegetables, you could add them to meals such as soups, casseroles, pasta, curries and salads.
Examples of vegetables and fruits are:
|
Vegetables carrots, leeks, courgettes, green beans, sweetcorn, cabbage, cauliflower, mushrooms, pumpkin, squash, sweet potato, aubergine, okra, asparagus and pak choi. |
|
Fruits apples, bananas, oranges, berries, pineapple, melon, figs, grapes, papaya, kiwi, peach, pear, plums, nectarines, rhubarb, mango, lychee, guava, jack fruit and raisins. |
Potatoes, bread, rice, pasta and other carbohydrates
Potatoes, bread, rice, pasta and other similar foods are known as carbohydrates. They are an important part of a healthy diet, and should make up just over a third of the food which you eat. Aim to include one food from this group at each meal. Try to choose wholegrain foods (brown rice or wholemeal pasta for example) if you can, as these contain more fibre, vitamins and minerals than white or refined starchy foods (such as white bread, rice or pasta). Wholegrains are also digested slower than white food, and so they give you more energy for longer, and you can feel full up for longer after eating them. Wholegrain carbohydrates include:
|
wholegrain breads, wholegrain pasta, wholegrain breakfast cereals, brown rice, skin on potatoes, whole oats, quinoa, plantain and yams. |
Dairy and dairy alternatives
Dairy foods are rich in protein and vitamins. They are good sources of calcium as our bodies can take the nutrition from it easily. Calcium is important for strong bones and teeth. To get the calcium you need, try to have three portions per day. Some dairy foods can be high in fat and saturated fat, therefore try to choose reduced fat, lower sugar and unsweetened versions where you can. If you are having food that is calcium rich but is not dairy, try to have ones that have calcium added, which are called Calcium enriched milk alternatives.
Examples of dairy and dairy alternatives are:
|
Dairy foods milk, yoghurt, cheese, crème fraiche, low fat cream cheese. |
|
Dairy alternatives rice milk, soya milk, oat milk, nut milks, coconut milk, and soya drinks, soya yoghurt, soya dessert, soya custard, soya bean curd/tofu (if set with calcium chloride (E509) or calcium sulphate (E516)), |
Protein
Protein is in meat, fish and meat alternatives (such as Tofu or Quorn). Some types of meat are high in saturated fat, which is not heart friendly, so try to choose cuts of meat that are lower fat. You can also remove skin and visible fat from meat and poultry, and try not to have too much processed meat. Examples of processed meats include sausages, bacon, cured meats and reformed meat products. You can also keep meat low fat by the way you cook it. Try to avoid frying in fat and opt for grilling meat and fish or poaching/boiling eggs. Fish is also a good protein source, and it is recommended that you have at least two portions of sustainably sourced fish per week, including a portion of oily fish. Beans, peas and lentils are also a good option because they are low in fat and high in protein, fibre, vitamins and minerals.
Examples of meat, fish and alternatives include:
|
Meats or fish chicken, turkey, lean beef, lean pork, white fish |
|
Oily fish mackerel, salmon, trout, sardines and kippers. |
|
Beans, peas and lentils kidney beans, butter beans, chickpeas, yellow split peas, red lentils, green lentils and puy lentils. |
Oils and spreads
It is important to have some fat in your diet, but most people have too much, in particular saturated fat. Eating too much saturated fat can make you at a higher risk of heart disease. Examples of saturated fat include butter, lard, ghee, suet, palm oil, coconut oil, processed meats, fatty meat, fried foods, takeaways, cakes, pastries and biscuits.
If you are worried about having too much fat, possibly because of having a high cholesterol or if you have been advised to lose weight, then try to include more foods which contain fats that are healthy for your heart. These are called unsaturated fats and they provide essential fatty acids and fat-soluble vitamins. Examples of these are:
|
Oils and spreads olive oil, rapeseed oil, corn oil, soya oil, sesame seed oil and nut spreads. |
|
Other sources of unsaturated fats: avocados, almonds, cashews, hazelnuts, oily fish, flaxseed, sesame seeds, sunflower seeds and walnuts. |
How do I know how much to eat of each food at each meal?
Keeping an eye on your portion sizes will help you to not eat too much at a meal or snack. Below is a guide to what a portion size is for different food types.
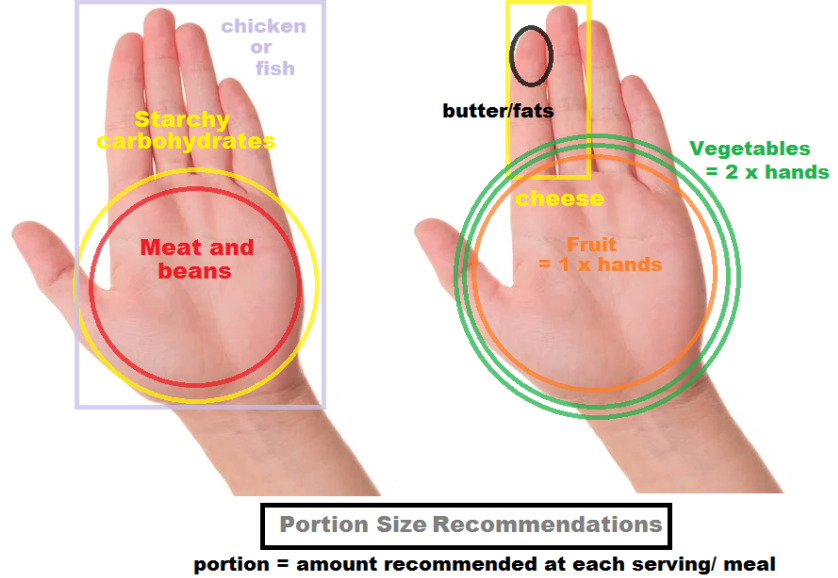
Reproduced with kind permission of the British Heart Foundation, a charity registered in England and Wales (reg. no 225971) and Scotland (reg. no SC039426).
How can food labelling help me choose the right foods?
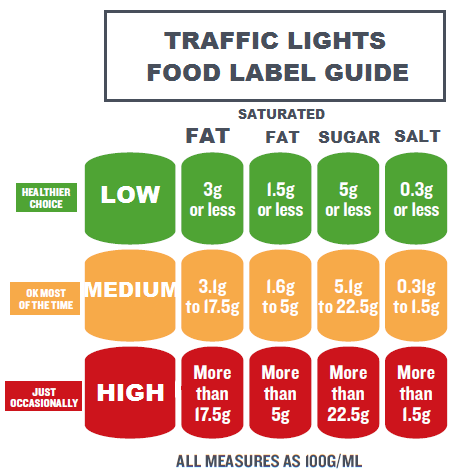
It can be hard to work out which foods are best for you, especially when you are food shopping. Foods that look healthy can be high in sugar, salt and saturated fat. You can use food labels to help you choose healthier foods. Many foods have information on the packaging which show a traffic light colour scheme. This means that by looking at the packaging you can see quickly if it is high in fat, salt or sugar. Red means that it is high, yellow means it is medium and green means it is low. The picture bellows explains this further.
How can I cut back on energy if I want to lose weight?
As you feel stronger and are able to do more and exercise, you may find that you want to eat more. This might mean that you put on more weight than you want to. If you have been advised that losing weight will be better for your health, here are some tips that might help you:
The best way to lose weight is to make sure you are eating a variety of healthy foods, from all the different food groups and making sure you are eating the right amount of food (so having sensible portions). A weight loss of 1 to 2 pounds (½ to 1kg) a week is a safe achievable target for most people
- cut down on sugary and fatty foods e.g. pies, pastries, cakes, biscuits, chocolate, and crisps
- plan ahead to help ensure you have the right foods available when you are feeling hungry (so you are not tempted to snack on high fat and high sugar foods)
- start the day with a healthy breakfast, such as fruit, yogurt, cereal, or egg on toast
- eat three meals, spread out throughout the day (and have low calorie snacks if you feel hungry between meals)
- shop with a list, so you are not tempted to buy foods you don’t need
- read food labels and check the fat, sugar and salt content
- aim to have 5 portions of fruit and vegetables a day
- half fill your plate with vegetables/salad and divide the other half between meat/fish/eggs/beans and a carbohydrate e.g. potatoes, bread, rice or pasta
- choose low fat spreads, salad dressings, sauces and dips and use small amounts of oils (olive, sunflower or rapeseed oil for example) in cooking if you drink alcohol, don’t drink too much, as alcohol is high in energy
- when you are eating away from home, make sure you don’t eat too much (as portion sizes can often be larger than you need)
- avoid eating at the same time as doing something else for example watching TV, that way you can concentrate on what and how much you eat
- eat slowly. It takes time for your brain to know your stomach is full so wait at least 5-10 minutes before having more
- ensure that you drink enough. Aim to drink 1.5-2 litres a day (3-4 pints). Try and drink plenty of water but you can also have some tea, coffee and low calorie soft drinks.
If you feel that you have lost muscle, it can help to still have a good amount of protein in your meals and drinks. Please see page 9 for tips about how to do this.
More information:
One You for how to get healthier and feel better:
Change for Life - Easy ways to eat well and move mor.
British Dietetic Association Food Fact Sheets have a variety of diet advice leaflets.
Websites with healthy and nutritious meal ideas: (remember to look at the serving sizes to work out the calorie, protein and fat content per portion).
Advice on to support you to start or continue to by physically activity:
- Chartered Society of Physiotherapy.
- Exercise on referral.
- NHS 10 minute workouts.
- Also consider using Apps like Couch to 5k, 7 minute workout, Fitbit, 30 day ab challenge.
See ICUsteps information for more information https://icusteps.org/information