The BDA’s Model and Process for Nutrition and Dietetic Practice (M&P) is an ideal framework for the measurement of dietetic outcomes.
The M&P requires ‘standardised language’ to enable outcome data to be collected in a systematic and straightforward way. The NHS has an agreed clinical vocabulary of standardised language terms (SL terms) known as SNOMED CT. In early 2022, specialist groups were invited to comment on the BDA’s lists of SL terms and to suggest new and updated terms.
In the summer of 2022, I was asked to work with the BDA to pilot the use of the updated SL terms when using the M&P and to evaluate their usefulness and effectiveness in providing sufficient and relevant outcome data.
In June 2022, I gave a webinar for BDA members entitled ‘A guide to creating PASS statements’, designed to support dietitians in using the M&P and in writing a clear PASS statement, as this is key to collecting relevant data on the outcome of dietetic interventions. The webinar is currently available on the BDA website.
I also gave a presentation at the BDA Groups and Branches Day in July 2022. This was an opportunity to encourage dietitians to join the pilot. A flyer was produced with the aim of encouraging participation from a wide range of different departments, teams, specialisms and settings. The pilot took place between August and November 2022, with 47 dietitians taking part, all working within the NHS.
The next stage was to develop the resources for the pilot. The Renal Nutrition Group agreed that their outcome tool could be modified for use in all dietetic settings. This tool incorporated the key parts of the M&P to enable the collection of the outcomes of dietetic intervention using lists of SL terms on an Excel spreadsheet.
The lists of SL terms had the following headings:
- Nutrition-related problem
- Aetiology
- Signs and symptoms
- Proposed outcome
- Outcome indicators
- Interventions Barriers
Key findings
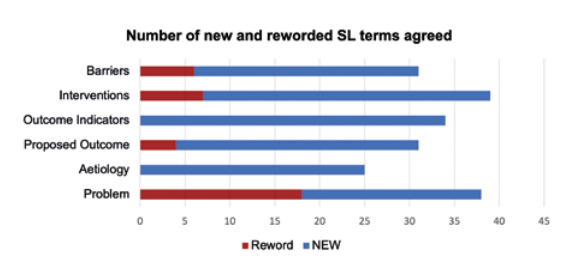
At the end of the pilot, all dietetic teams were asked to complete an evaluation through an online survey and comment on the SL terms (on Excel). Questions focused on the SL terms’ usefulness and effectiveness. They were asked for their suggestions as to any new or amended SL terms that they would like to add to the tool for future use, as well as any terms to delete. In total, 14 teams completed the evaluation, representing 47 dietitians from most geographical regions within England and Scotland based in acute and community settings and covering adults and paediatrics.
M&P and PASS statements
The survey found that two thirds (64%) of teams “always” or “usually” used the M&P in their clinical practice. Fewer than half of the respondents (43%) “always” or “usually” wrote a PASS statement (43%). Seven per cent were “extremely confident” in writing a PASS statement, with 50% “quite confident”. Nearly two thirds of teams (64%) agreed that their level of confidence in writing PASS statements had increased by the end of the pilot.
Standardised language terms
There was generally good agreement that there were sufficient SL terms to meet their needs and most agreed that the SL terms were relevant.
Comments included:
“The main issue was people being overwhelmed with the number of terms, although once we went through a few specific examples and they had some time to look through them it became easier and more familiar.”
“The current terms look good/sufficient for certain areas. However, [we] need additional options added for other specialties.”
Nearly two thirds (64%) agreed or strongly agreed that the SL terms helped them to be more effective at writing PASS statements and evaluating outcomes.
Most respondents wanted to keep the majority of the SL terms, with some suggestions for rewording due to terms being outdated and not reflecting current practice and terminology.
Outcome tool
Forty-four per cent felt the Outcome tool was an “extremely” or “very” useful way to demonstrate dietetic outcomes. Over half (61%) felt that it was an effective way to demonstrate dietetic outcomes.
Nearly half found the tool difficult to use, the main difficulty being the length of time needed to choose the most appropriate SL terms and having to enter the data on a spreadsheet rather than within the content of the outcome tool itself.
Over 60% felt that the outcome tool enabled dietitians to prove their worth.
Comments on what could be improved included “Having a standard template to complete for documentation” and “Making it easier to input data integrated into NHS systems used”.
Discussion
Dietitians found it hard to suggest SL terms for deletion, yet many commented that there were too many. Lack of familiarity with the terms meant that dietitians often found it difficult to choose the most appropriate term from a long list. Confidence grew as dietitians became more used to the lists of SL terms over the three-month pilot.
Despite many suitable SL terms on SNOMED, there are still significant gaps. As M&P is not yet used by all dietitians in all clinical areas, there is a lack of knowledge and confidence on how to write a PASS statement and how to use SL terms meaning updated SL terms will need further refinement over time.
It was recognised that only a small number of dietitians were recruited to take part and therefore the results may not have accurately reflected the overall opinion of dietitians throughout the UK. To counter this, opinion from specialist groups was sought to review and refine lists further.
| CATEGORY | NEW STANDARDISED LANGUAGE TERM | COMMENTS |
| Problem/ aetiology | Unable to meet nutritional requirements orally | |
| No enteral route for nutrition | ||
| Poor tolerance of enteral nutrition | ||
| Excessive nutrition-related medication | For use when considering medications as well as diet eg cystic fibrosis, diabetes, kidney disease | |
| Imbalance of nutrition-related medication | ||
| Inadequate nutrition-related medication | ||
| Weight stigma | To encourage use of preferred weight-related Living with obesity terminology | |
| Living with obesity | ||
| Moderate malnutrition | Using GLIM criteria | |
| Severe malnutrition | ||
| Limited access to food | ||
| Outcome indicators | Energy intake (% of requirements) | |
| Protein intake (% of requirements) | ||
| Refeeding profile | ||
| WHO wellbeing questionnaire | Validated tool for wellbeing | |
| Weight bias internalisation scale | Understanding self-directed stigma | |
| Dietetic intervention | Dietary education on modification of infant formula | |
| Dietary education for carbohydrate counting | ||
| Dietary education for fluid allowance | ||
| Nutrient dense diet | ||
| Advice provided to prescribe nutrition borderline substances | To enable advice regarding ACBS-approved borderline substances and advice re nutrition-related medication to be captured | |
| Recommend to change prescription of nutrition-related medication | ||
| Medication commenced by NMP (nonmedical prescriber) | For supplementary prescribers |
Examples of new SL terms
Taking this one step further
New standardised language terms
Discussions were held with the Chair of the Obesity Specialist Group to ensure we use the preferred weight-related terminology such as ‘living with obesity’ to minimise weight stigma. There were also discussions regarding the use of Global Leadership Initiative on Malnutrition (GLIM) definitions for malnutrition. Other SNOMED terms required updating to ensure person-centred language such as using “concordance” or “adherence”, rather than “compliance”. Further terms were added relating to motivation, confidence and behaviour change.
Global Leadership Initiative on Malnutrition: a framework for diagnosing adult malnutrition
GLIM is a new framework for diagnosing malnutrition in adult patients. It includes five practicable indicators that can be used in routine clinical practice. Both moderate and severe malnutrition are diagnosed using this framework.
Weight-related terminology including weight stigma
How healthcare professionals communicate with people living with obesity impacts engagement, motivation and the relationship between the service user and the healthcare professional. Experiencing weight stigma is associated with lower wellbeing and reduced motivation to engage in health-related behaviours.
Weight stigma refers to negative attitudes and beliefs that devalue people based on their weight status that may include bias, discrimination, stereotyping and social exclusion and, whilst experienced by people of all weights, it is mostly directed towards people living with obesity.
The positive impact of changes in standardised language should demonstrate respect for the service user, enable clear communication and facilitate the capture of dietetic outcomes.
The updated list of requested new and reworded terms will be sent to NHS Digital in early April 2023 and, if approved, will be added to SNOMED and will be available on the BDA website.
Next steps
A further project is underway to investigate the feasibility of a unified dietetic digital record. The aim will be to develop a core dietetic record template embedding the updated SL terms on SNOMED within. This means that the recording and evaluation of problems, interventions and outcomes can be undertaken seamlessly. To undertake this work, it is vital that I am able to link in with individual dietitians, dietetic managers, first contact practitioners and digital champions to assess the feasibility and the practicalities required to enable a suitable template to be devised.
If you are interested in joining a round table discussion as our first step or in offering your expertise or experience in any other way, please email [email protected].
The benefits to the dietetic workforce would be that both the M&P and the digital record are aligned and that up-to-date SL terms will facilitate both the clarity of dietetic records and straightforward collection of both outcomes and impact of dietetic intervention, helping us to prove our worth.

